This long post will be a summary of what we have learned so far about the Coronavirus, and I’ll make some predictions about what to expect next. Since I’ll be sharing so much information, I won’t give references for everything here. I also have to make the disclaimer that new studies are constantly being done, and some of the below information may need to be revised later. To make my standard disclaimer, I am not an epidemiologist or a physician. I have a Ph.D. in molecular biology, and my specialty is infectious disease testing. On much of the below, I have an informed but not expert opinion.
Coronaviruses: Coronaviruses are a large group of viruses unrelated to the flu. What we think of as the common cold, are actually member of several classes of viruses like Adenovirus, RSV viruses, Rhinovirus, and several Coronaviruses. Many Coronaviruses cause diseases no more virulent than the common cold. However, just like novel flus can cause extra trouble, so can novel Coronaviruses. The first SARS virus was much more lethal that the SARS-2 virus, but because SARS had a short incubation period and made almost every infected person sick, it was much easier to contain. The Middle East Respiratory Syndrome (MERS) Coronavirus infects a few people every year, and is very lethal, with a fatality rate of 34%, but it also has not made a global impact. The reason SARS-2 is so dangerous is that it’s VERY infectious (Ro of between 2.5 and 5.7) and has a VERY long incubation time (2-14 days), making it very hard to track. Plus, it’s at least 2x as deadly at the annual flu.
Name: The official name of the virus is SARS-2-CoV (for Severe Acute Respiratory Syndrome-2 CoronaVirus). The official name for the disease it causes is COVID-19 (for COronaVIrus Disease-2019). You may notice that the term SARS actually sounds a lot like a disease. You would be right. So why did they need a different disease name than SARS-2, or SARS-19? I don’t know.
Origin: Controversy over the origins of the SARS-2 virus began very early in the pandemic. The most common theories were that the virus arose naturally at a live animal market in Wuhan China, where animals from a wide variety of species are sold. The predominant theory is that the SARS-2 virus arose in bats, then transferred to another animal, perhaps a pangolin, before moving to humans. This has been the most accepted theory for the majority of the pandemic, promoted by the WHO, the CDC, and American media.
The lab leak theory, the idea that the virus arose from the Wuhan Institute of Virology, was present from the beginning, but was heavily disfavored by official channels for most of the pandemic. On May 23, 2021, the Wall Street Journal published an article that gave evidence for idea, followed closely by an article from Vanity Fair. The articles normalized discussion of the theory and as of this writing, polls show that a majority of Americans believe that the virus came from the WIV.
Emails between several virologists, public health officials and Dr. Fauci strongly suggest that this group believed that the virus may have come from the laboratory as early as January 31, 2020. However, this same group published a scientific article on February 9th supporting the natural origin theory. The paper was at odds with discussion in the email correspondence. If investigations show that the group published claims they knew to be false, this would represent a significant case of scientific fraud.
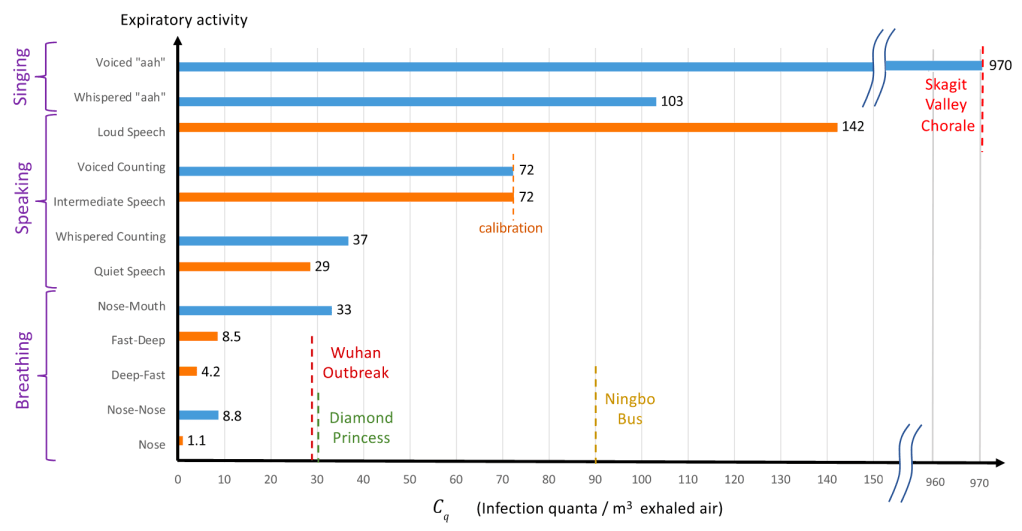
Spread: Early reports were that SARS-2 mostly spread like a flu, with droplets spreading from coughing or sneezing. It became apparent later that the virus was also spread through aerosols by laughing, singing, shouting, or even just talking in close proximity for long periods. As further study was done, it appears that most infected people don’t infect anyone else. Rather, most infections come from “super-spreader” events, in which a single person infects a large group of people. This usually happens indoors (at least 19 times more likely) during activities like fitness classes, funerals, concerts, and choir practices. While outdoor activities aren’t completely immune to these events, outdoor transmission of SARS-2 appears to be extremely rare.
Viral load upon exposure appears to be an important determinant of how severe a case will be. Basically, this means that if you’re infected by a “low dose” of virus, your disease is likely to be less severe. I have several physician friends who have stated that it seems to them that cases in the hospital are less severe than they used to be. One likely reason for this is that since more people are wearing masks in public than early on, those who are infected are being infected by a lower viral load.
Early studies demonstrated that viable viral can exist on objects for hours or days. However, it does not appear that a substantial number of people are being infected because they have touched a contaminated object.
The WHO made a confusing claim that asymptomatic people cannot spread the virus. While this is technically correct, they were not clear that “asymptomatic” is a technical medical term meaning someone who does not have, and will never have, symptoms. Another group is “pre-symptomatic”. These are people who currently don’t have symptoms, but will develop symptoms in a few days. As it turns out, pre-symptomatic people do spread virus, and are likely responsible for up to 80% of new cases. So yes, people without symptoms can and do pass the virus to others.
Risk Factors: Many believe that only old people are at risk. While it’s true that age is a dominant factor, other risk factors are important, and younger people have also experienced severe symptoms. Other risk factors include:
age
asthma or COPD
heart conditions
kidney conditions
liver disease
high blood pressure
diabetes
obesity
auto-immune disease
use of NSAID anti-inflammatory medications
being immunocompromised (HIV infected, undergoing cancer treatment, under medication for a transplant)
vitamin-D deficiency
type A blood (Type O appears to be protective)
inadequate sleep
Always check with your doctor before changing your medications. I have an auto-immune disease and take daily anti-inflammatories, but my doctor has advised me to continue taking these unless I experience COVID symptoms. Make sure your doctor is aware if you have any of the above conditions.
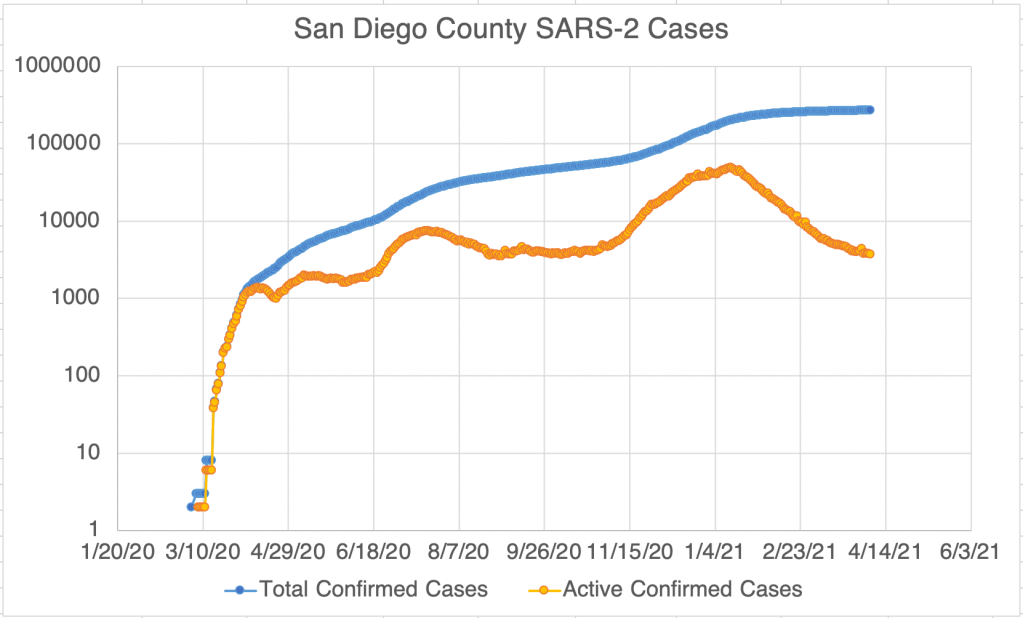
Symptoms: Many people who have SARS-2 experience no symptoms, or experience mild flu symptoms. If you have ANY cold or flu symptoms, contact your doctor and see if you can be tested. If you live in San Diego County, and your doctor cannot offer you a test, call 2-1-1 to get a free test from SD County Public Health. If you have additional symptoms like shortness of breath (you just can’t seem to get enough air), loss of smell or taste, nausea or diarrhea, contact your health care provider or an urgent care immediately.
In severe cases, the virus can do wide spread and permanent damage to multiple organ systems. Early treatment is necessary to prevent the most severe symptoms.
Precautions: While lockdowns may have been effective in the US during the early stages of the pandemic, especially at a time when masks were hard to come by, recent evidence suggests that lockdowns provide only a moderate benefit over other means of control. Here’s what appears to be beneficial:
Masks: Masks are not all the same and some are better than others. Their main benefit is that they stop, reduce, or slow the travel of virus from infected people. This prevents surrounding people from infection or lowers the viral load of exposure. N95, KN95, and KF94 respirators are effective at filtering close to 95% of virus. A good mask is well fitting and filters the air moving in an out of your mouth and nose. The commonly used surgical masks and other loosely fitting masks do not filter air and I don’t recommend using them.
Social Distancing: Aerosolized virus can travel through the air. Staying 6 ft away from others helps prevent infection. Social distancing may be more important for droplet transmission, like the flu, than for aerosol transmission in which microdroplets can stay suspended for much longer and travel much further.
Handwashing:
Adequate sleep: Sleep is very important for a wide variety of body functions, including the immune system. Get 7 – 8 hours of sleep per night. A 26 minute power nap during the day is also beneficial if needed.
Vitamin D: Several studies have suggested that patients with the most severe cases of COVID also have the lowest levels of Vitamin D. Because of our often indoor lifestyle, most Americans are Vitamin D deficient to some degree. The best way of getting some Vitamin D is to make it yourself by going outside in shorts and a T-shirt for 30 minutes a day. This is because Vitamin D is manufactured in our skin in response to sunlight. If it’s not practical for you to do this, consider a Vitamin D supplement. Darker skinned people are more likely to be Vitamin D deficient in the US. Supplementing Vitamin C and Zinc is also recommended.
Home isolation: If you have cold or flu symptoms, contact your doctor immediately and see if you can get a test. Tests are much more available that early in the pandemic, and you should be able to get a test by request. Also, if at all possible, isolate yourself from the rest of your family until you can be tested as negative. Many new infections are taking place among family members.
I’ve been traveling all over the country, and have been in dozens of airports, gas stations, and stores. I get tested regularly and have always been negative. Here are the precautions I use:
1) Wear a mask or face covering indoors in public. Now that vaccines are available, I no longer avoid unmasked people indoors, but as an unvaccinated person, I still wear mine.
2) Keep 6 ft away from others. (I basically ignore this one if other precautions are in place, especially on an airplane!)
3) Avoid indoor gatherings, especially ones in which singing or shouting is likely. This is now voluntary now that we have vaccines, as an unvaccinated person, I still follow this rule.
4) Outdoor gatherings are fine, even without masks, if everyone maintains a distance. I have hosted several outdoor gatherings.
5) While many restaurants are open for limited indoor seating, I personally am still not comfortable eating indoors at a restaurant. I enjoy eating outdoors at restaurants, however.
6) Wear an N95 or KN95 mask when going to more high risk areas like airports or public areas where people may gather. These masks are rated to filter out 95% of viral particles. In my opinion, surgical masks and especially neck gators are nearly worthless in these settings.
7) I never take my mask off on the plane, and find an isolate spot in the airport to eat or drink on layovers.
Vaccinated people can relax many of these rules! Vaccines are 90-95% effective, so you still have a small chance of infection.
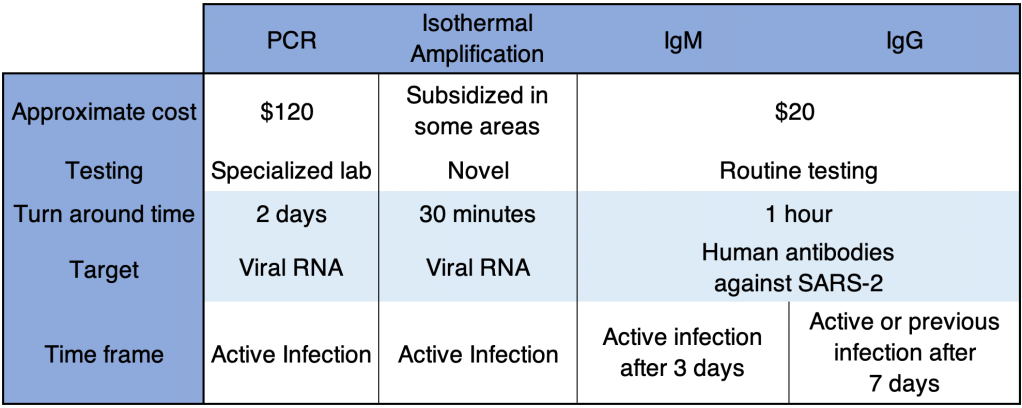
Testing: There are several kinds of tests, and they tell you different things.
PCR: These tests use material collected from the nose and need to go to a specialized laboratory for processing. They are very sensitive and specific, and indicate whether the patient is currently infected. This is the most common kind of test. They can take longer to process because they need specialized equipment that most small labs don’t have, so most of the wait time is just for shipping to a specialized facility.
Antibody: These tests detected antibody from a patient’s blood to see if the patient has been infected for at least a few days. IgG tests may also tell if a patient was infected weeks or months previous, but are no longer infected. Some patients do not mount an immune response that will provide long term antibody. These tests are cheap and fast, but are more prone to false positives and false negatives than PCR tests.
Antigen: These tests use a very similar technology to Antibody tests, but instead of detecting a patients antibodies against virus, they use antibodies to detect viral proteins in a sample. An “antigen” in immunology lingo is just a protein that can induce an immune response. So in this context, an “antigen” is a SARS-2 protein that can be bound by an antibody. Like PCR tests, these tests detect an active infection, because they detect viral proteins currently in the body.
Isothermal amplification: The Abbott ID Now COVID tests uses this relatively new technology. These tests are similar to PCR but more prone to false negatives.
If you have cold or flu symptoms, contact your doctor immediately and see if you can get a test. Testing is much more available than it was early in the pandemic. San Diego County is encouraging anyone who wants a test to be tested.
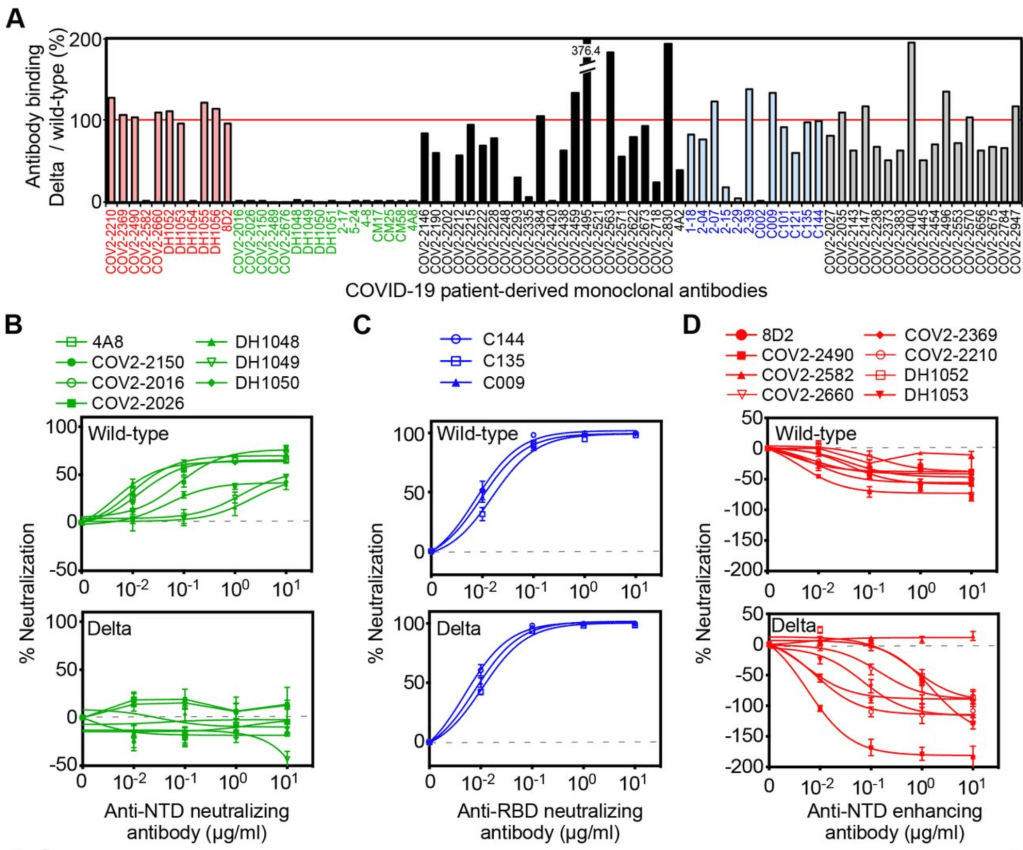
Antibody Dependent Enhancement: I’ve written about this a lot and I won’t describe it in depth here. In short, this pathway allows some viruses to create more severe disease on the 2nd time infecting a person than the first. It is theoretically possible, perhaps even likely with SARS viruses, which is why I have been careful to avoid infection and why I’m not going to get the vaccine unless perhaps my work requires it.
Treatments: Treatment for COVID is complicated and not all patients can be treated in the same way. Additionally, treatments are evolving rapidly, and your doctor many not treat you in the ways listed below.
Supportive care: Most treatment is supportive care, treating symptoms while the patient recovers naturally. Anti-inflammatory medications are often used to prevent the immune system from over-reacting to the virus.
Ventilators/nasal cannula: While widely used early on, some doctors now state that ventilators carry risks that may be unacceptable for COVID patients. Many doctors now favor oxygen therapy using a nasal cannula, using ventilators only as a last resort breathing if labored.
Remdesivir: This antiviral was used widely for much of the pandemic, but many sources now claim it has limited effectiveness.
Dexamethasone: Steroid used to treat patients with low oxygen levels.
Hydroxychloroquine, Azithromycin, Zinc: Several doctors from several countries have reported success with this combination. Studies on the effects of these drugs have as yet still been non-conclusive. Some positive studies suggest that Zinc is the main virus fighter of the treatment, with Hydroxychloroquine allowing better penetration of Zinc into cells. Unfortunately, the debate on the efficacy of this regimen has taken on a strongly political tone, which almost always interferes with the scientific process. Now pundits, as well as scientists, weigh in on this regimen. Treatment with Ivermectin is likely more beneficial in a wider range of disease state than HCQ.
Ivermectin: A anti-parasitic medication used since 1981, Ivermectin has reportedly been used by doctors around the world, notably India and Mexico, to reduce COVID fatalities. Reports claim that Ivermectin is beneficial in a wide range of disease state, from pre-disease prevention to late stage disease. Like Hydroxycholoroquine, promising data was often labeled “misinformation” by outlets in Western countries, and western doctors were strongly discouraged from prescribing it. Thus, experimentation with Ivermectin was hindered and the drug’s potential is still unknown.
Vaccines: Each spring, scientists learn which flu is likely to be prominent by the following Fall. They make some guesses and create a vaccine for the flu season. The manufacture process takes a few months. But it’s only this short because they already know how to make a flu vaccine. Development of a brand new type of vaccine takes between 4 and 30 years! There are many methods to make a vaccine, and scientists must try many of them before finding one that works. Then they must try the vaccine on patients and make sure they are relatively safe. Every vaccine carries some risk of side effects.
Several vaccines against SARS-2 were finally released to the public in December of 2020. The vaccines released to the public are in 2 types:
Attenuated vaccine: This type has been commonly used for decades for a variety of viruses. The technique makes a severely weakened form of the virus that still makes viral proteins that provoke an immune response. With this type of vaccine, the patient is infected by a weak form of the virus that they quickly recover from, usually with no symptoms other than occasionally the flu like symptoms that are your body’s natural response to invasion.
mRNA vaccine: This is a brand new technology that has been worked on for years. The SARS-2 vaccines are the first ones that have been introduced to the public using this technology. The vaccine includes a piece of mRNA inside a lipid bilayer that mimics the cell wall. The mRNA is inserted into the cell where it is translated into a copy of the viral Spike protein. These vaccines are 90-95% effective against infection, and even those infected have less severe symptoms. However, they are not 100% effective, so some infections of vaccinated individuals has occurred.
As has often happened, the vaccines have generated significant controversy. As you know, I have been careful to avoid being infected and also getting the vaccine because of the potential of ADE. My concern with the vaccine actually has nothing to do with the new mRNA technology, I actually have no reservations about the mRNA vaccines. From an ADE perspective both the attenuated vaccines (Johnson & Johnson) and the mRNA vaccines (Pfizer and Moderna) produce Spike protein that may trigger an ADE response should a new strain of SARS virus appear, not a variant, a new SARS strain, like a “SARS-3”.
When the vaccines were released, rumors of side effects, sometimes severe, arose immediately. For some time, I minimized these as a risk of any vaccine. All vaccines carry the risk of side effects and even death. However, a video podcast featuring Robert Malone, the inventor of mRNA vaccine technology, convinced me that the Spike protein itself has toxic properties of its own, separate from the vaccine technology used. This is because the Spike protein can bind to cells all over the body and may have wide ranging effects.
Despite ADE and issues with side effects, I actually still believe some will benefit from the vaccine. These include the following groups:
Anyone over 60
Anyone with 1 or more risk factors:
obesity
certain auto-immune diseases
use of NSAID medications
heart, lung or kidney condition
immunocompromised patients (HIV, cancer and transplant patients)
respiratory condition such as asthma or COPD.
Frequently working with the public
Musicians who sing in indoor settings
Medical personnel
Again, I am not a physician, so check with your healthcare provider while making decisions about getting the vaccine or changing your medication.
If you’ve had the vaccine or had COVID and are concerned about ADE, remember that it will only become a factor if a significantly new strain arises (“SARS-3”). If this happens, then the procedure for you would be to be very careful initially, then get the “SARS-3” vaccine as soon as possible. The new vaccine will protect you from the new virus. In the future, vaccines against Coronaviruses will be produced even more quickly than this time.
The vaccines have pros and cons. I’m in support of vaccines for some but not necessarily for others. Each person needs to weigh the risks for themselves. I am not for companies or government agencies coercing individuals to get the vaccine.
Herd Immunity: The idea of herd immunity was popularized in pre-pandemic discussions on vaccines, promoting the idea that the more people are vaccinated, the more protection for those who can’t be. The idea is useful, but in my opinion, efforts to push people into getting vaccinated to achieve herd immunity are misplaced. Before a vaccine is available, the only way to reach herd immunity is to expose large numbers of people to the virus, which is counter productive. Now that the vaccine is available, those who are concerned should just get the vaccine themselves and not harangue others about getting it. Gentle persuasion may be convincing, but haranguing rarely is. Given even the pre-pandemic resistance to vaccines, a forceful effort to vaccinate is likely to back-fire.
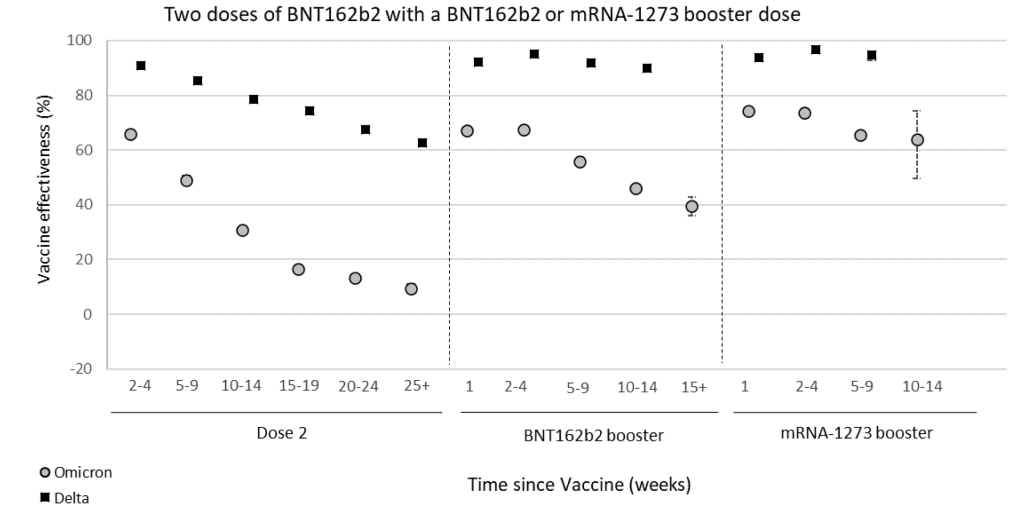
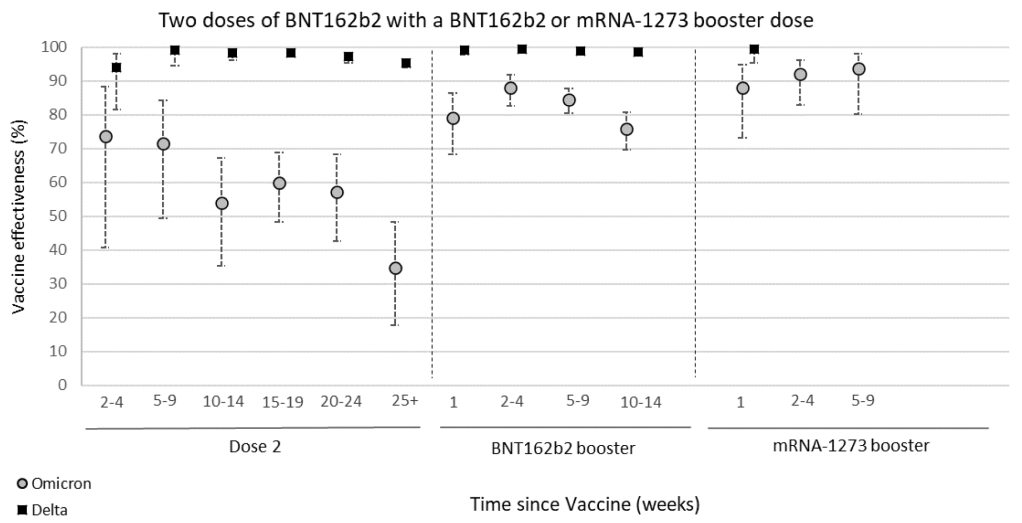
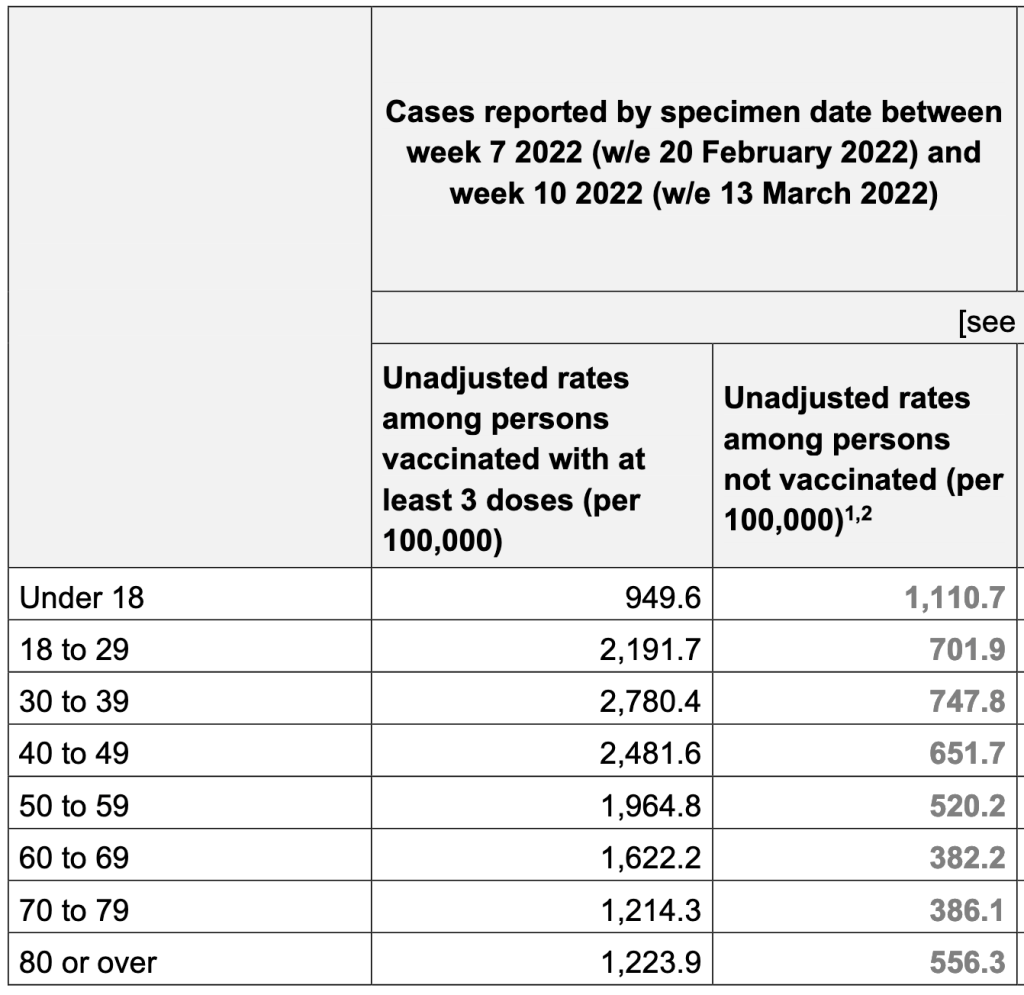
Variants: During the course of the pandemic, several variants have arisen that have a slightly different Spike protein sequence from the original Wuhan strain. Confusingly, naming conventions have changed several times, making it difficult to keep them all straight. As a general rule, the variants have all been more infectious than the Wuhan strain, but have not been more pathogenic. Fortunately, the vaccines have been effective against all of the variants, although are not as effective against some variants.
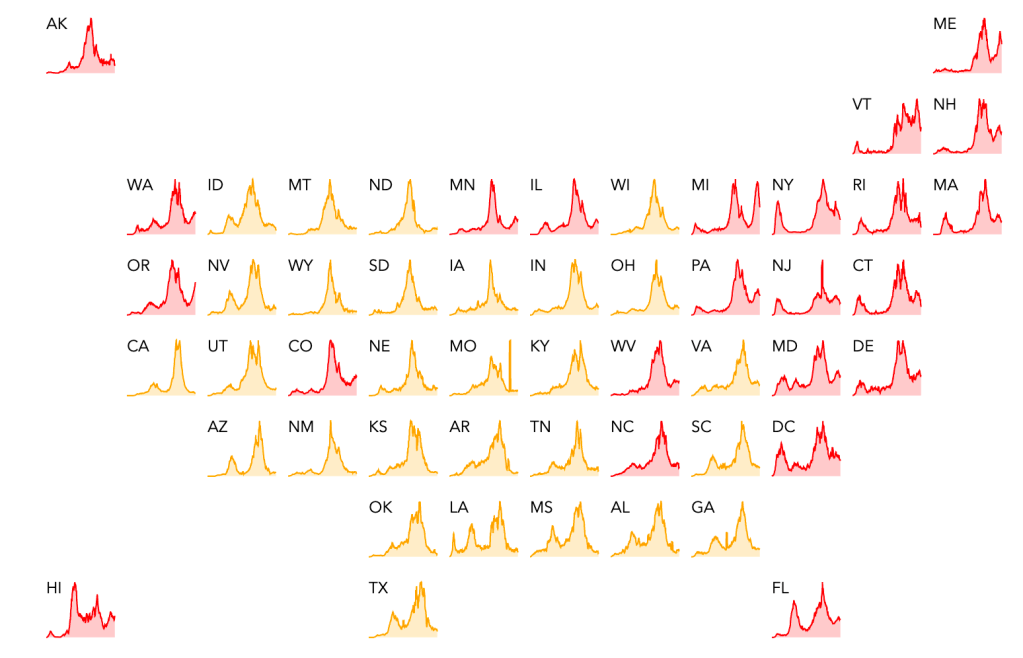
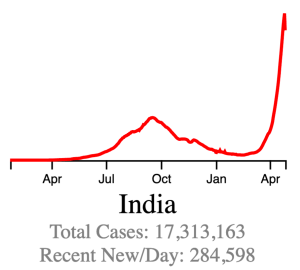
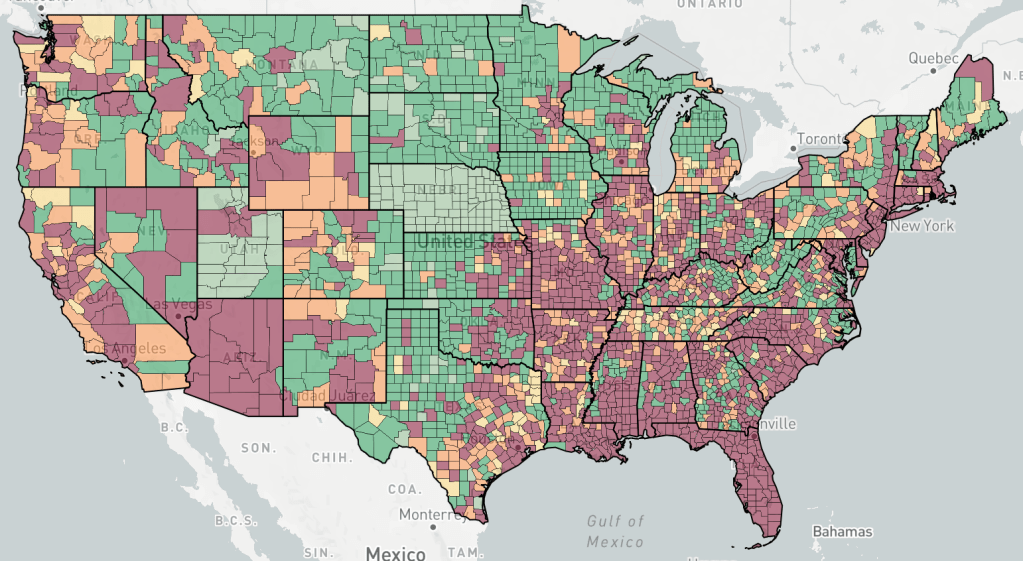
The Delta Variant: The UK/Alpha variant caused waves of new infections in some countries and was more infectious than the original Wuhan strain. In late 2020, a new variant arose in India, the India/Delta variant. This variant was significantly more infectious than other strains and has caused huge peaks in cases in several countries. As of this writing, several countries are still experiencing waves of new cases most likely due to the Delta Variant, including the United States.
While the Delta Variant has caused large numbers of new cases and an increase in hospitalizations, data suggests it may be less pathogenic than the Wuhan or UK variants.
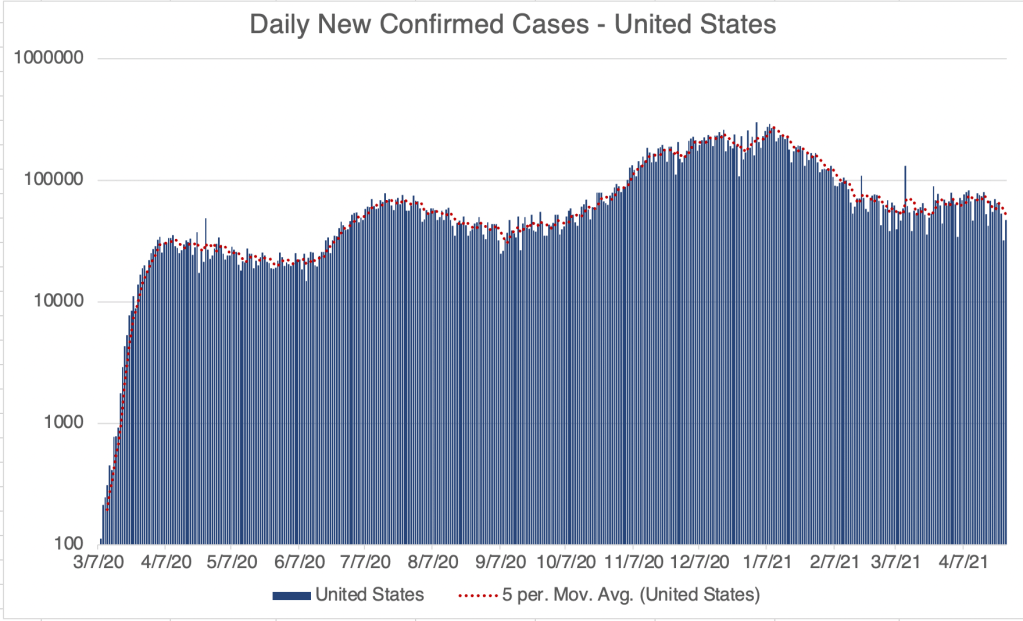
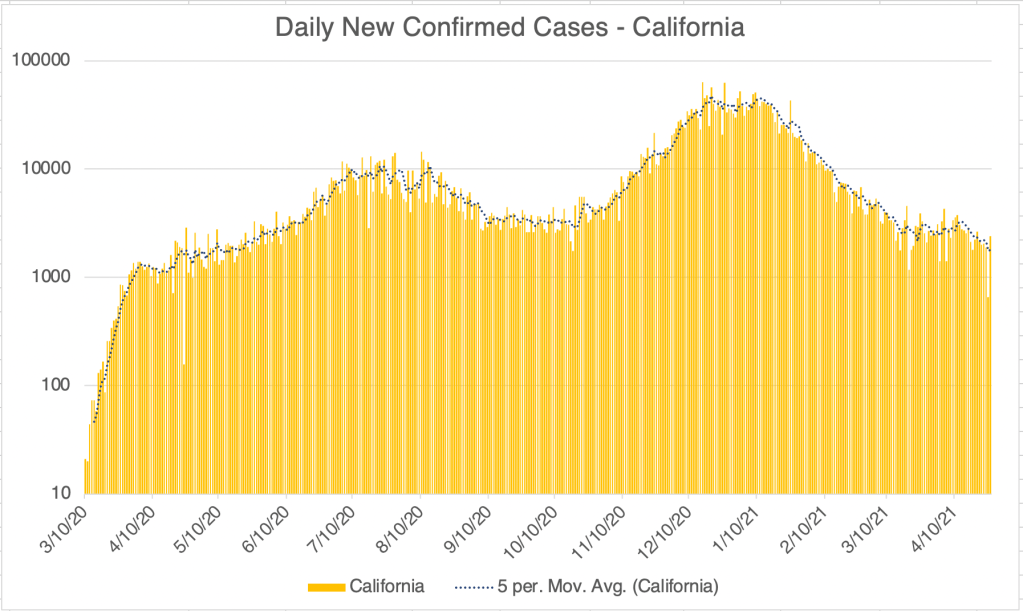
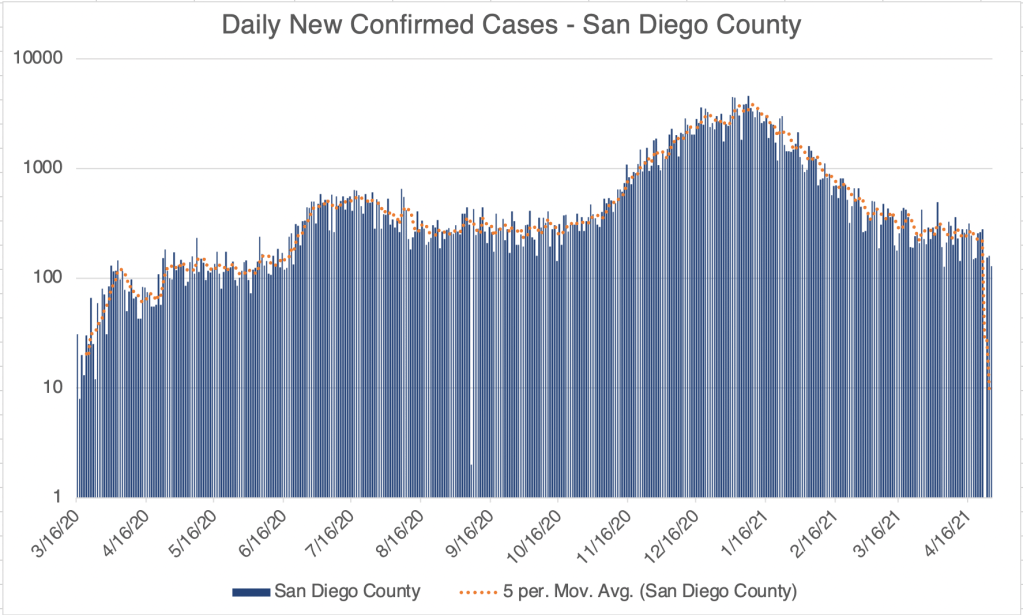
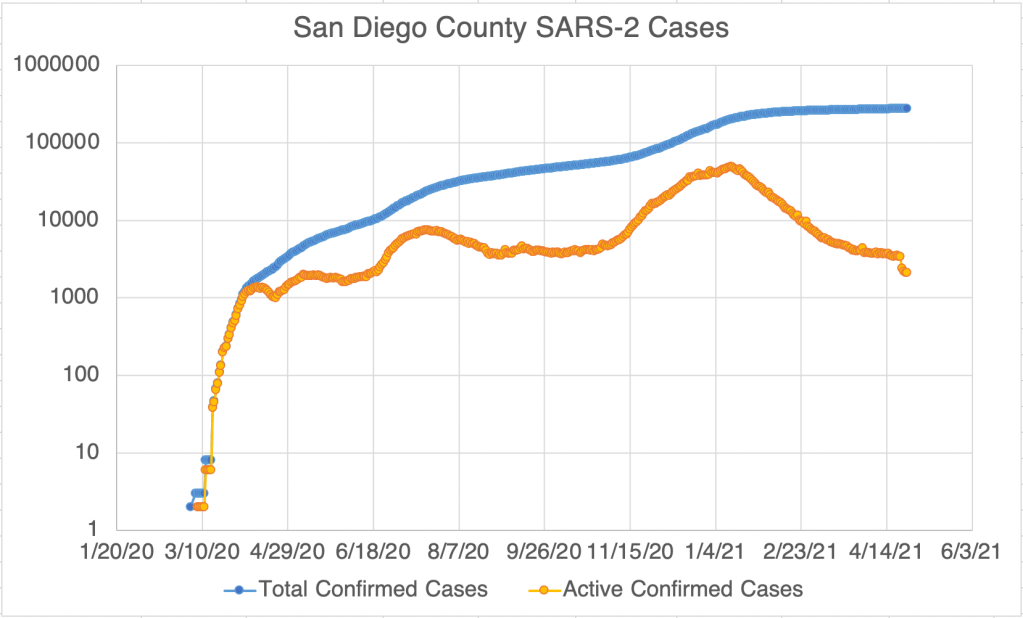
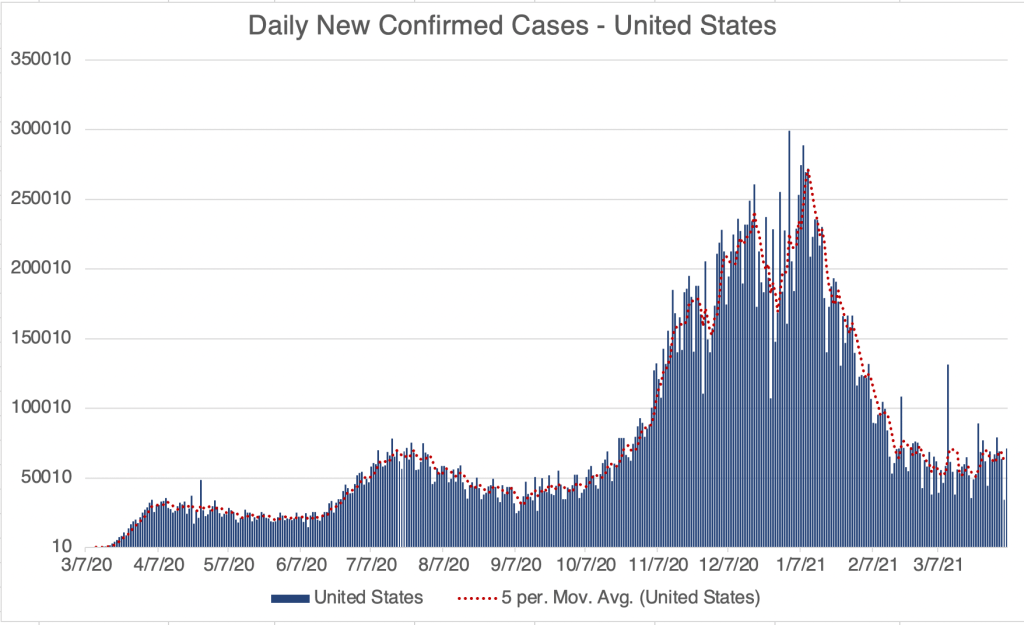
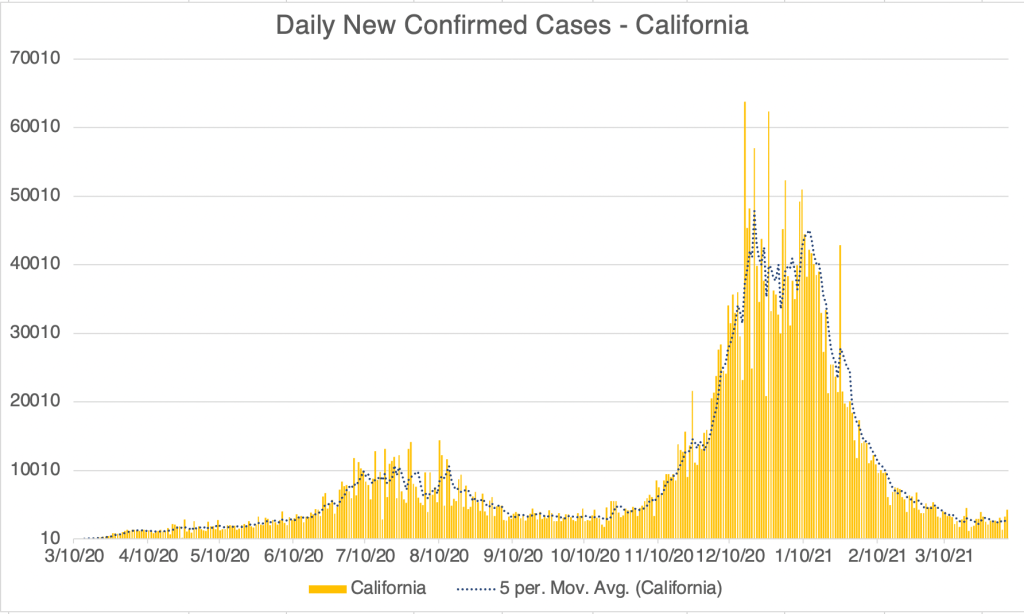
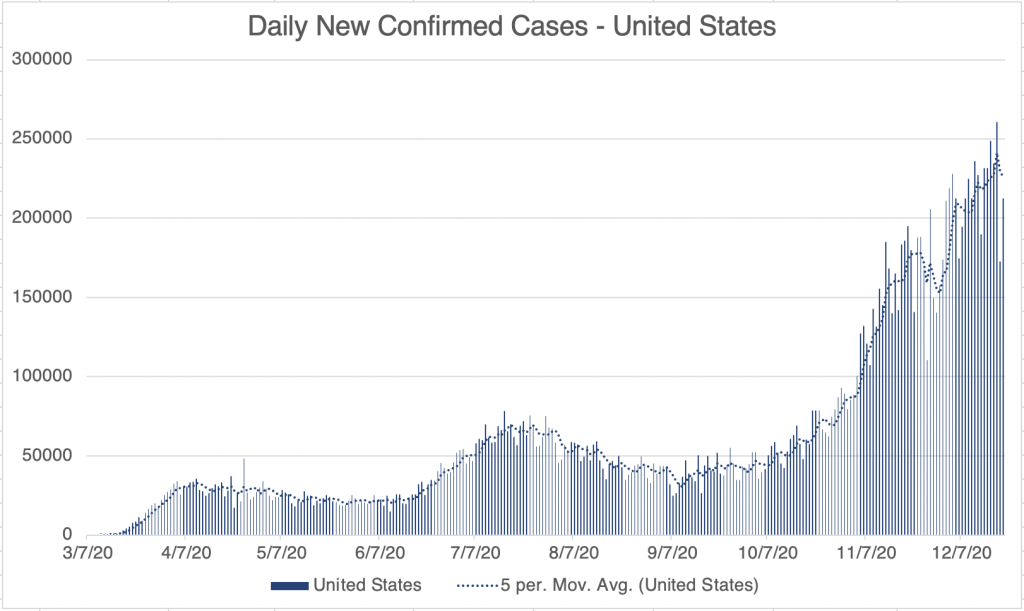
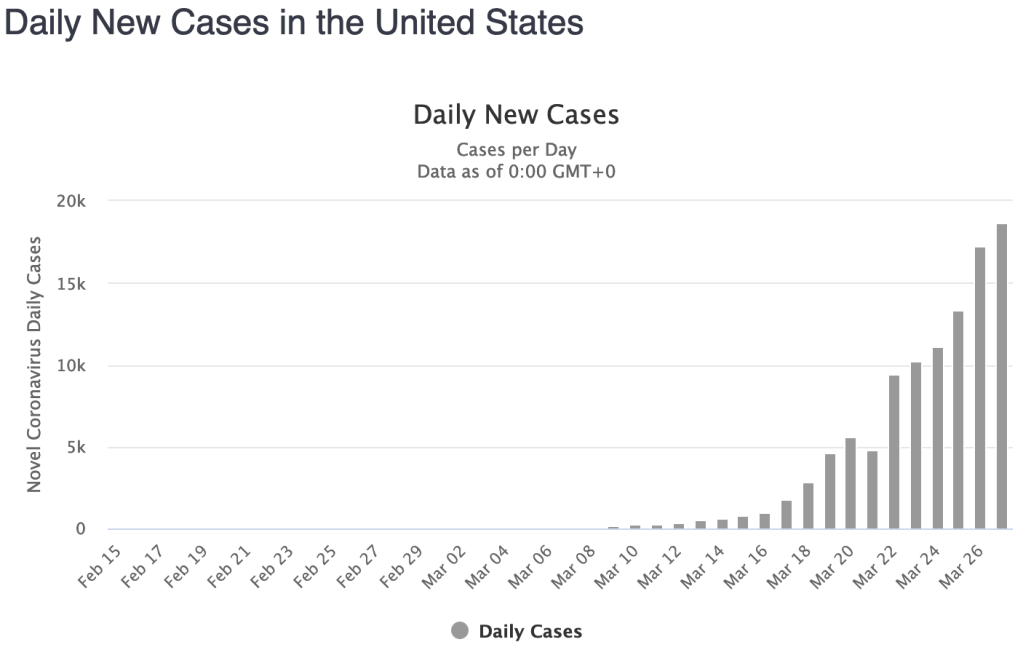
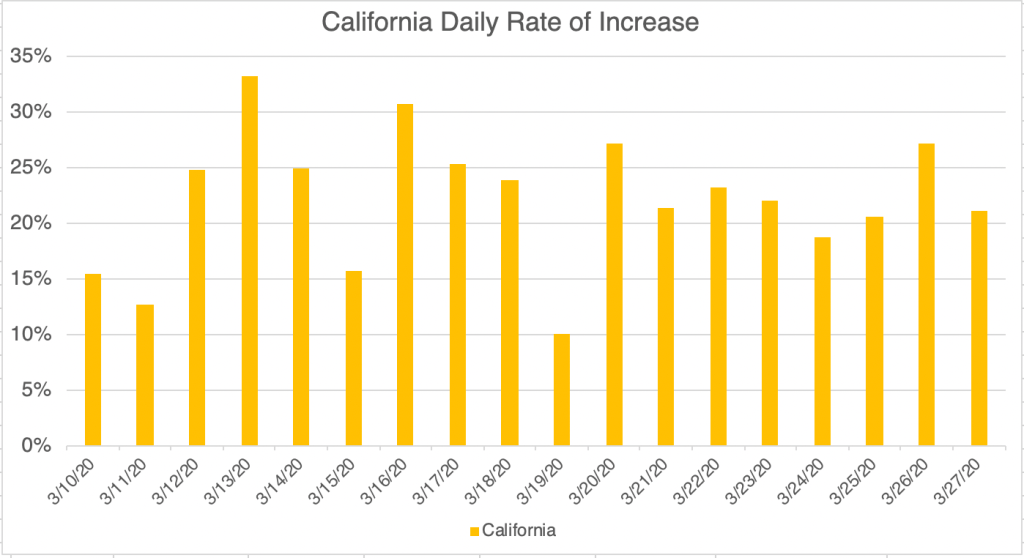
Current Status: In late Spring, at least in the US, life began to get back to normal, with approximately 50% of the US population vaccinated, much lower new case numbers, and reduced restrictions. Currently however (July 21, 2021) a wave of infections, likely caused by the Delta variant, is causing concern and some calls for new restrictions. Several other countries scattered across the globe are also currently experiencing peaks in cases.
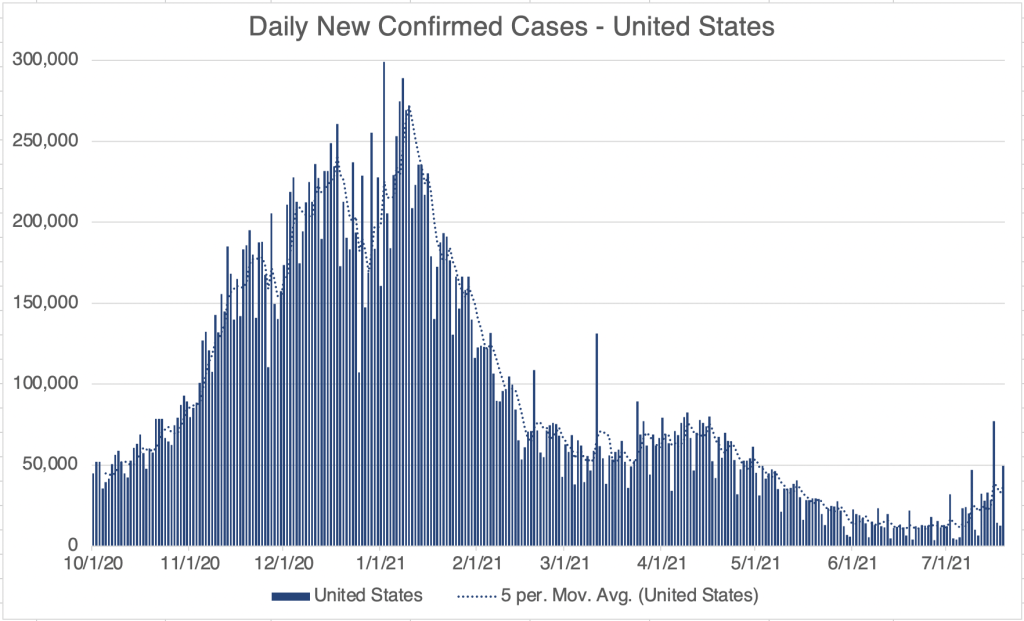
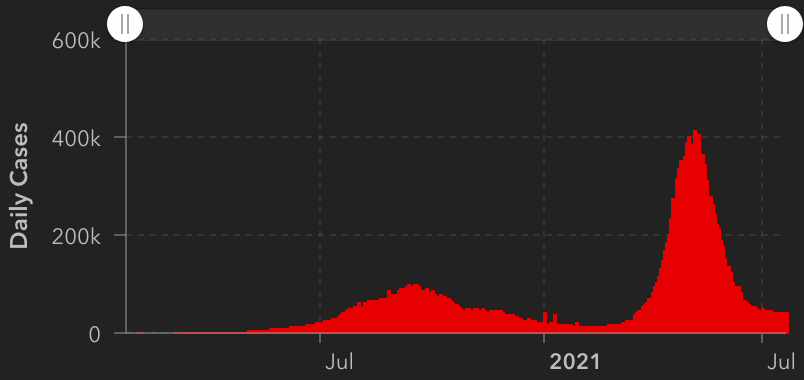
The Future: Since vaccination started in the US, there have been many fewer new cases. This has led many to basically go back to behaving normally. The Delta Variant is rightly causing concern, but I’m still hopeful that the current peak in new cases will be short lived. In other countries with Delta related waves, the peak has been very sharp, with quickly increasing, then quickly decreasing case numbers. However, I’ve started to be a little more cautious in public again, while we wait for the increase in cases to slow.
Several other countries are still experiencing an elevated case load. The pandemic won’t be truly over until cases are low in all countries. I’m hopeful that this will happen this year, but it’s certainly too early to know for sure. So far, all new variants have been susceptible to the vaccines and natural immunity. There is a small chance however, that we may see new versions that are not. If this happens, SARS may become endemic, circulating seasonally like the flu does. So far, I don’t see evidence that this will happen.
In the future, we may have a “SARS-3” a new virus from the SARS family that will be similar, but different enough to trigger the ADE pathway. If this happens, those of you that have had COVID or been vaccinated should be very careful to avoid infection initially, then get the “SARS-3” vaccine as soon as it is available.
In a future post, I’ll give my recommendations for what should be done differently if a new pandemic should arise.
Don’t fear, but be smart,
Erik