Note, March 26th, 2022: The first part of this post was written on July 7th, 2020. Since that time, there has been evidence that appears contradictory in the ADE story. Reading the entire post will help you understand how ADE and COVID are related, but it is a complex and evolving issue, so things may still change.
Originally posted July 7th, 2020
I’m going to bring up an issue that I’ve been avoiding talking about for some time. I’ve been avoiding talking about it because it’s not a certainty, and also because the possibility will be scary for some. The reason I feel compelled to talk about it now is that many are having a hard time understanding why I am still so concerned about the virus when the fatality rate is low and dropping, and folks want to get back to normal life. I’m even hearing about young people having COVID parties in which people gather with a sick individual so they can all get infected and be immune from the virus thereafter.
Before I share this, I’ll also say that the medical community is doing a better job treating patients with COVID, and the disease is becoming more survivable. In addition, we now know a lot about how the virus is spread, and if a person wants to remain uninfected, they can do that, while still getting together with friends and family, and still working and getting on with life. You can be reasonably certain you will not get infected if you do the following:
1) Wear a mask or face covering in public. Avoid places with unmasked people.
2) Keep 6 ft away from others.
3) Avoid indoor gatherings, especially ones in which singing or shouting is likely.
4) Small outdoor gatherings are fine, even without masks, if everyone maintains a distance. Have guests bring their own food.
5) While many restaurants are open for limited indoor seating, I personally am still not comfortable eating indoors at a restaurant. I enjoy eating outdoors at restaurants, however.
Antibody Dependent Enhancement: Several years ago, scientists were developing a vaccine against Dengue Fever, a mosquito borne disease which causes debilitating joint pain in patients. Some time after trial vaccination, several vaccinated patients died suddenly of Dengue Fever. This became the most studied example of Antibody Dependent Enhancement (ADE). Normally, for the annual flu let’s say, a person gets infected by the flu, is sick for a few days, and the immune system develops a response by creating antibodies against that specific strain of the flu. If they are exposed again in a month, nothing will happen. If the patient is exposed to a different strain the following year, they may still get sick, but the antibodies they developed the year before may help them have less severe disease and recover more quickly. Part of the immune response is that some immune cells display antibodies on their surface to capture new invaders.
With Dengue and some other viruses, the first stages are normal. A person gets infected and develops a response. If they get re-infected a month later, nothing happens. But if they get infected with a slightly different strain months or years later, instead of being protected, the virus attaches to antibodies displayed on immune cells and uses the antibodies as a site of entry into the immune system. The immune system is quickly infected, and the patient has a more severe disease with the second infection. Some estimates are that disease may be 3-4 x more severe in these patients.
As it turns out, SARS-1, which arose in 2002, and MERS, which has small outbreaks every year, are both Coronaviruses and both appear to be able to use the ADE pathway. This raises the possibility that SARS-2, the current virus, can also use the ADE pathway. This means that a person infected for a second time with a different strain of SARS-2, or any other Coronavirus for that matter, may be at much higher risk for severe disease.
This is why I’m not in favor of pursuing herd immunity as a pathway out of this crisis, because it will prime people for ADE related problems if a similar strain should strike next year.
This is not a new idea. If you search for “ADE” or “Antibody Dependent Enhancement”, you will see many articles, some peer reviewed from respected journals, on the phenomena. Dr. Fauci has even referenced it using the term “enhancement” when talking about vaccine development.
Why haven’t the government public health departments been more open about this? They tend to make statements only based on what they can be reasonably certain of, which is why they have been so slow to react to many aspects of the current crisis.
Again, it’s not certain that ADE will play a role next year. It’s too early to know. I’m informing you of the possibility so you can make wise decisions for you and your family.
_________________________________________
Update: November 20, 2020
Since writing the above post, things have changed a little. There have been a handful of known cases of people being re-infected with SARS-2. In some of these patients, symptoms were worse, while in others, symptoms were less severe. In all of the well characterized cases, the 1st and 2nd strains that infected them were different, suggesting that it’s not a re-infection by the same strain, but a new infection by a different strain.
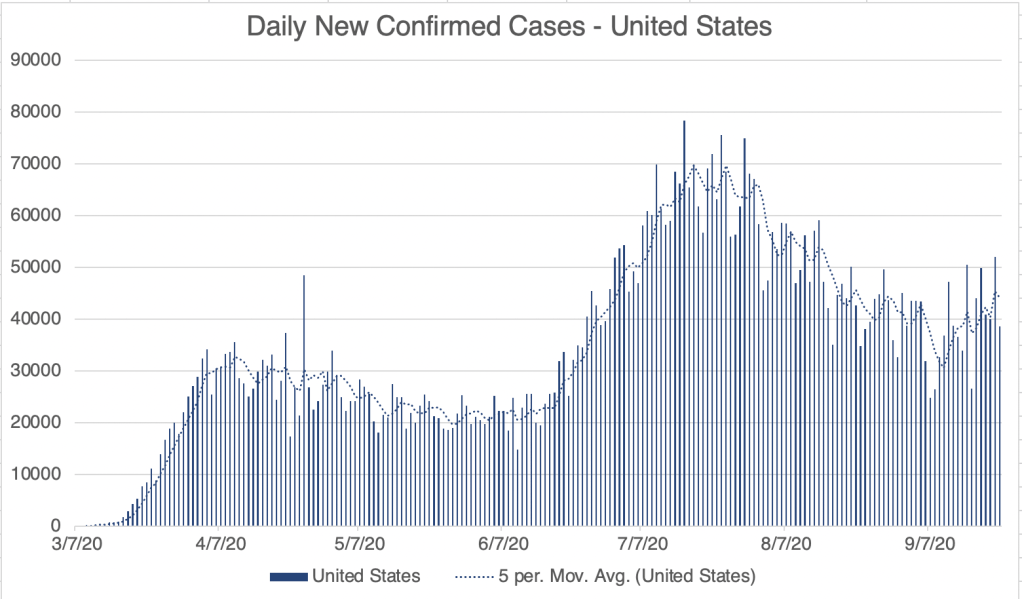
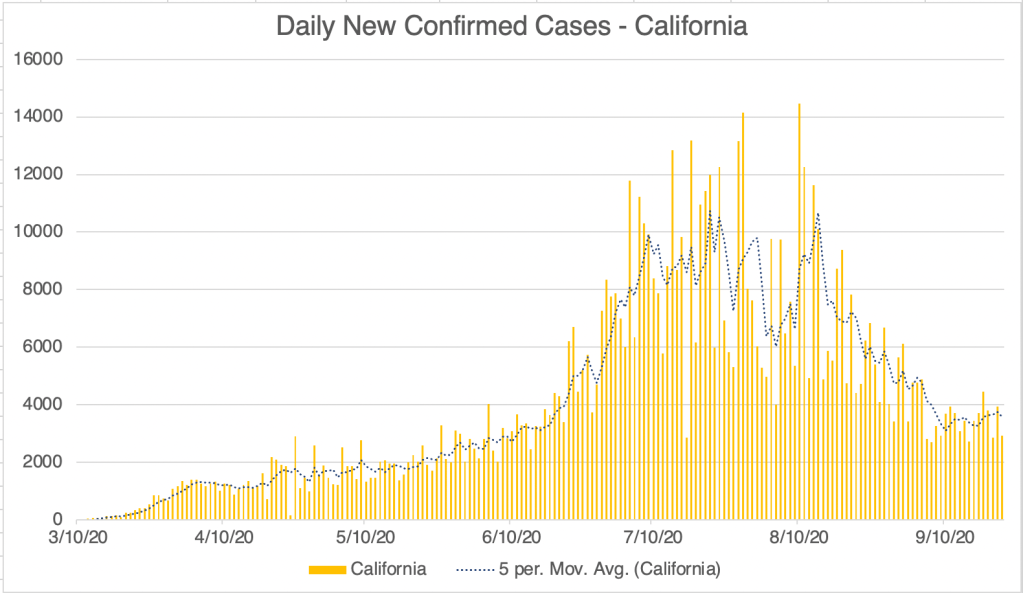
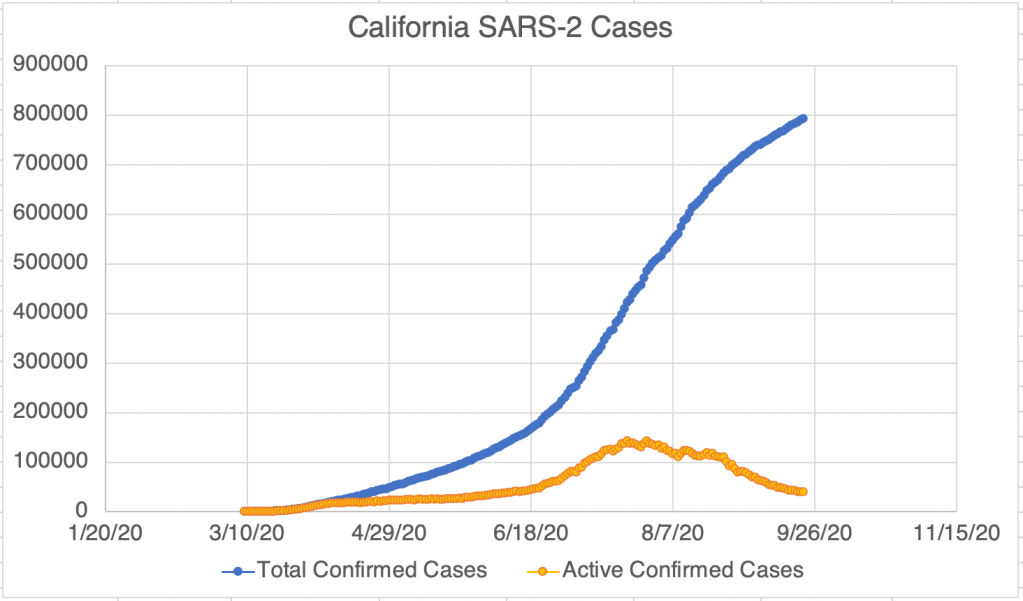
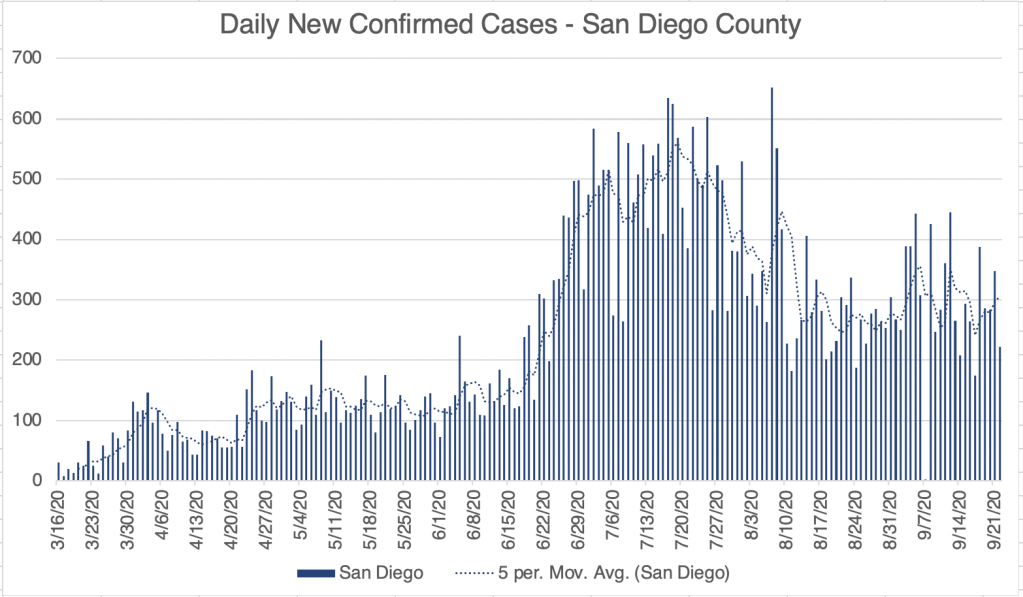
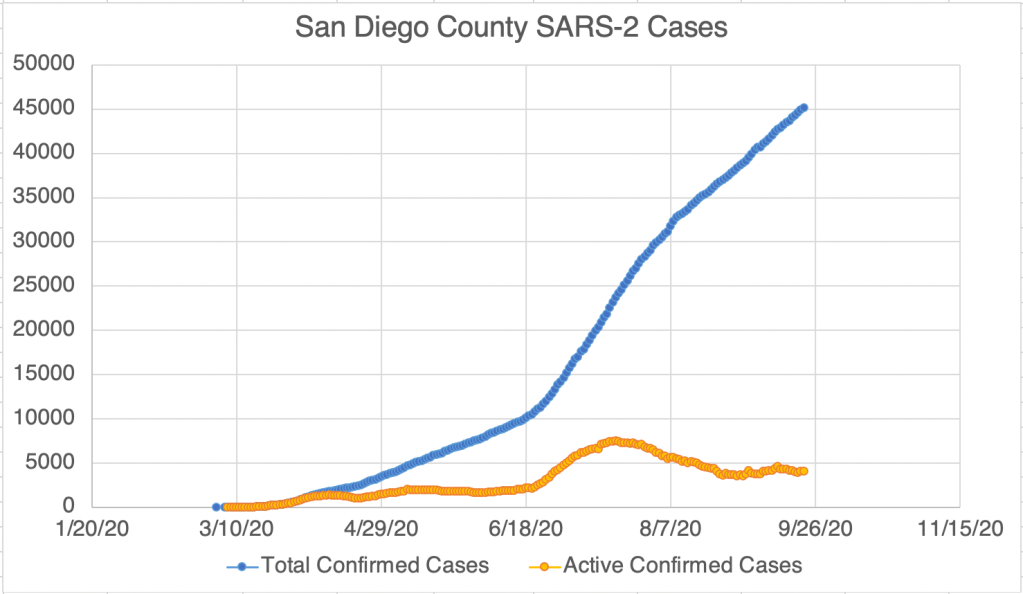
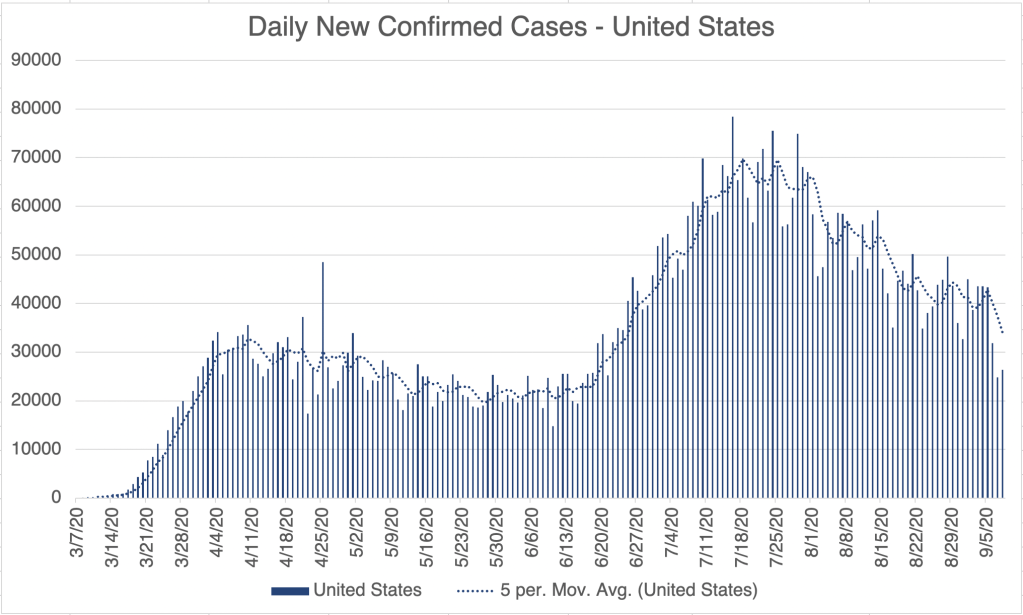
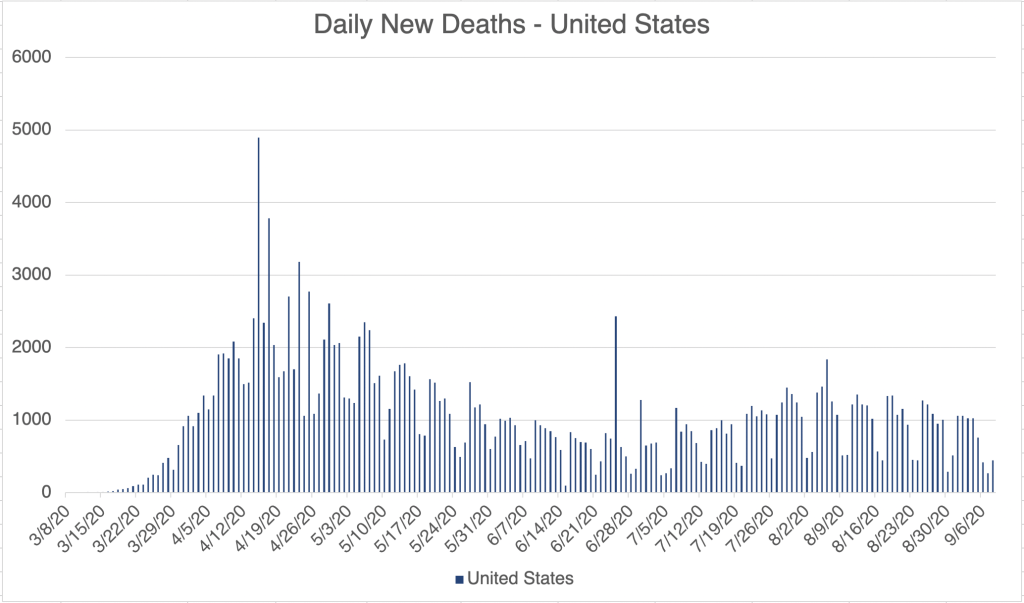
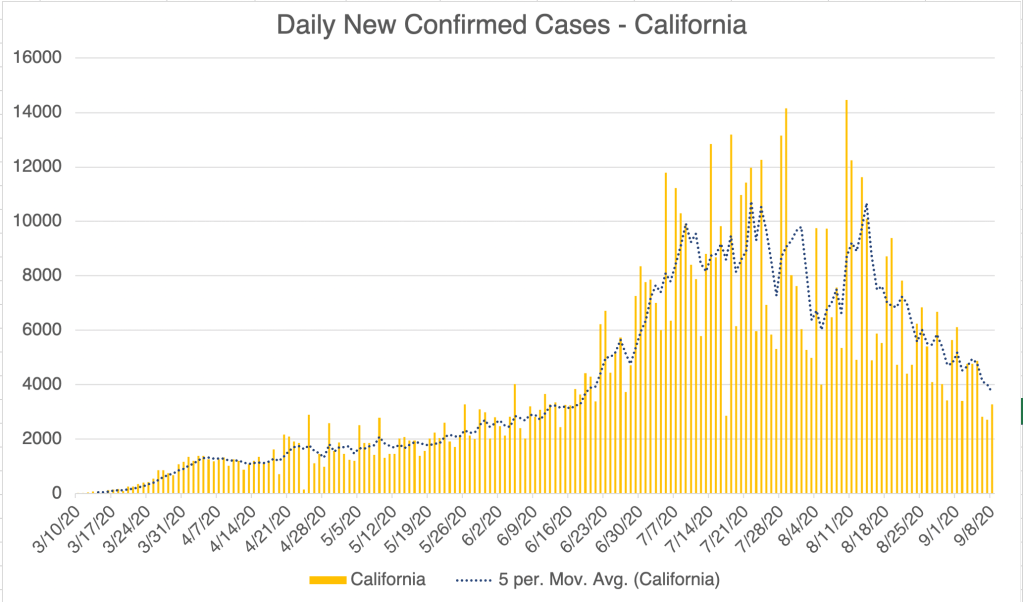
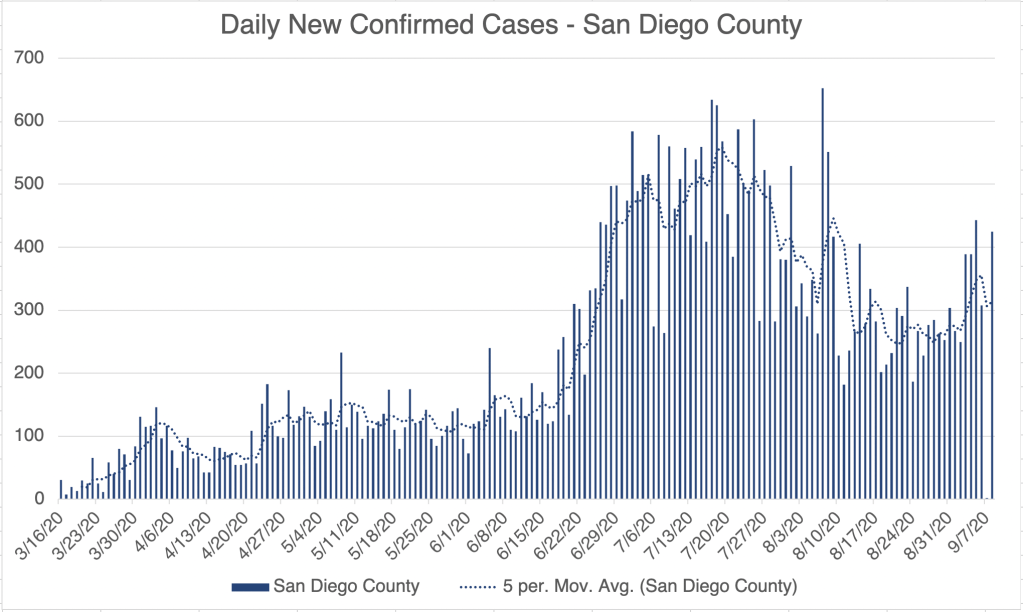
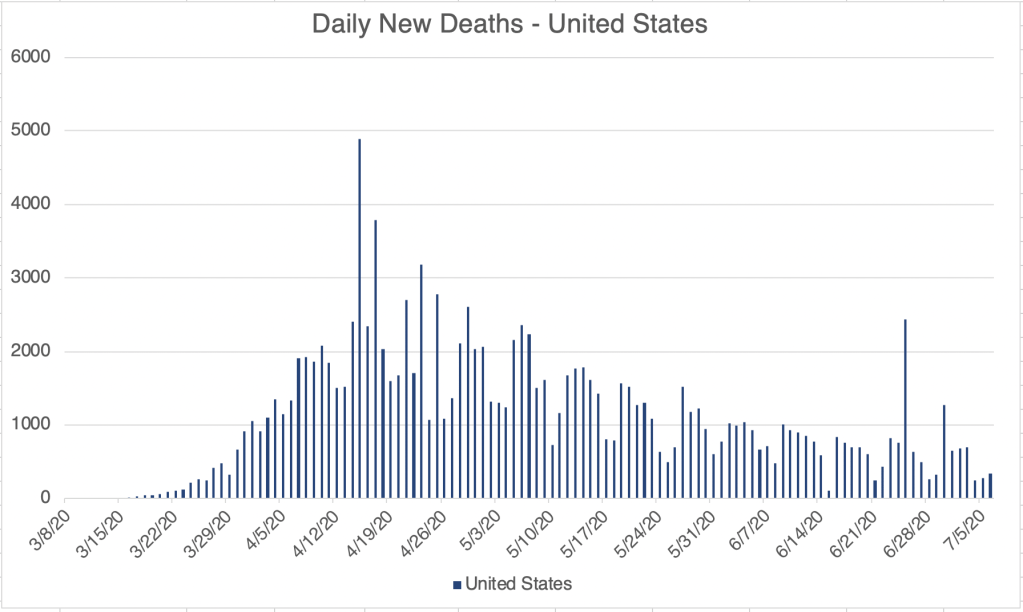
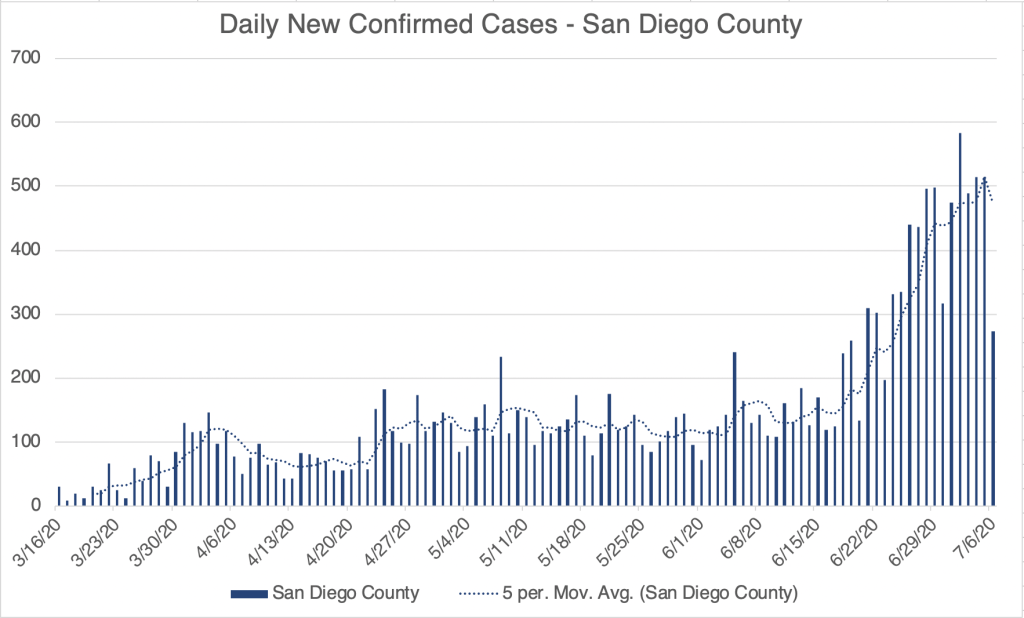
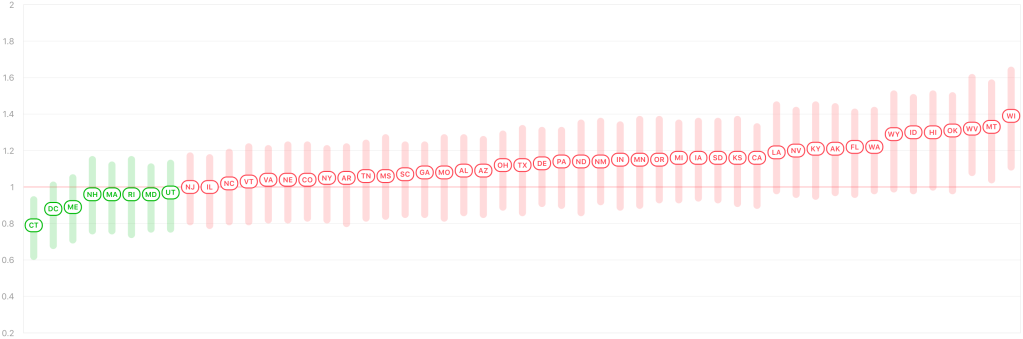
We’ve had at least 2 main strains in the US, SARS-2 which arrived in January or February, and a strain called D614G which probably arrived in April or May and likely caused the 2nd wave in June and July. The D614G strain is likely more infectious than the original SARS-2 strain, but is perhaps less virulent, since the fatality rate during the second wave appears to have been lower. In fact, there may have been several strains circulating around the world and the US for much of the pandemic.
How does this all relate to ADE? The fear with ADE is that a 2nd infection will cause worse symptoms than with the first infection. This may still be true. But we’ve had several circulating strains and so far, no real evidence the re-infections have universally been worse. So it appears for now that the ADE experiment is already going on, and that perhaps the phenomena will not have as great an impact as I feared. I am currently cautiously optimistic that ADE will not cause significant additional mortality.
This also has some impact on the vaccine discussion that is currently ongoing. If ADE will not have a significant impact, than the vaccine may be safer that I previously thought, and I have become cautiously optimistic about the success of the vaccine.
_________________________________________
Update: December 12th, 2020
More on ADE and Vaccines: Some potential very good news for me on the vaccine front. For months I’ve been warning about ADE, the phenomena that some viruses can be even more dangerous in a second infection than the first. Karen Parrott, a former colleague at Quest Diagnostics, often provides me with interesting COVID related stuff. This week she sent me a podcast featuring Paul Offit, the developer of the first Rotavirus vaccine and an author of many books on immunology and vaccine production. I am not an immunologist but he is. More importantly, he’s the first authoritative person that I’ve heard in the media speak at length on the ADE issue and how it relates to COVID. He claims in the attached clip (time stamped at 14:40) that the current vaccines do not appear to trigger the ADE pathway in animal models, and human trial subjects never displayed the signs that ADE was involved in secondary exposures. This difference from SARS-1 and MERS may be related to the fact the SARS-2 is much less virulent than these other 2 viruses.
This makes me more optimistic that the vaccine will be safe from an ADE perspective. I won’t be able to get the vaccine for some time, but I am more willing to get it now than ever before. Several physicians I know are eager to get it as soon as it is available. This is great news!
In the interest of full disclosure, I will point out the some patients receiving the vaccine the UK have experienced some injection site irritation, especially in those with allergies. This is actually somewhat normal for vaccines, and appears to pass within a few days.
Now that mRNA vaccines have been produced for the first time, future development of this new kind of vaccine should be even faster than this time!
________________________________________________
Update: April 13th 2021
ADE and the next SARS virus: I wanted to explain a little more about my continued concerns about ADE. As the pandemic progresses and we have numerous variants circulating around the world and the US, ADE does not appear to have had an impact on the current situation. This is certainly good news. If it did have an impact, we would be seeing additional deaths from the new variants, which we do not.
My continued concern comes because ADE impacts our ability to fight the NEXT virus. SARS viruses (SARS, MERS, SARS-2) have the ability to easily infect the immune systems of those previously infected with closely related but different strain of the virus. If a future strain of SARS comes out, let’s call it SARS-3 for now, ADE may become a big deal. I stress that this is only theoretical at this point. SARS was moderately infectious, but also very pathogenic, giving all known patients severe symptoms and killing 10%. It was actually less dangerous globally, since outbreaks tended to be detected early and quickly snuffed out. SARS-2 is highly infectious, but much less pathogenic. It’s greater global impact came from it’s very high infectiousness and very long incubation time, being passed even from pre-symptomatic patients. The tendency of all viruses is to become more infectious and less pathogenic over time, a pattern followed by SARS and SARS-2. If we have a SARS-3 someday, it will likely be even more infectious than SARS-2, but less pathogenic. On the other hand, MERS is more pathogenic than SARS, so this pattern doesn’t always follow. The next time another SARS coronavirus breaks out, we will need to be very careful initially until we understand the parameters of the new virus.
So what do you do if you had COVID or had a COVID vaccine if a SARS-3 comes out? If that happens, vaccine production will likely be much faster than this time. Be very careful with the virus initially, and get the new vaccine as soon as it is available to you, because you may be at greater risk for severe symptoms. I know some of this is confusing and counter-intuitive! Feel free to ask questions below!
Update: August 30th, 2021
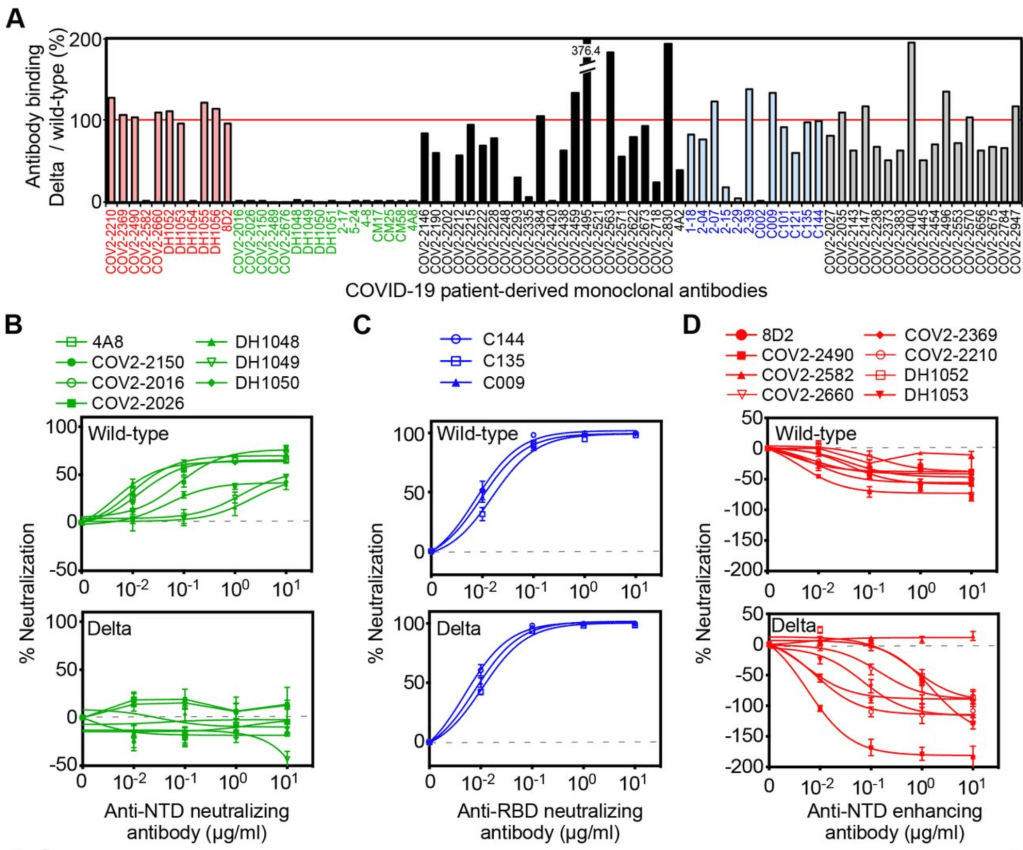
Delta already using the ADE pathway? A doctor friend of mine sent me a pre-print paper from a lab in Japan. Please note, this is a pre-print paper and has not yet finished peer review! The paper describes experiments using antibodies derived from patients infected with the Wuhan strain, as well as with the Delta Variant. They then studied binding of these antibodies to artificial viruses. The paper argues that Delta variant viruses are less neutralized by vaccines against “wild-type” or Wuhan strain vaccines. While the “wild-type” antibodies against Wuhan can neutralize a region of the Delta Spike protein called the Receptor Binding Domain (RBD) (Figure 1C), other antibodies binding to another region of Delta Spike protein actually enhance infectivity. Figure 1D from the paper shows negative levels of “neutralization” for antibodies that bind the N-terminal domain of the Spike protein. The paper calls this “enhanced”. Yes, this is the ADE I’ve been talking about.
They suggest that with rapid changes in COVID variants, a new version of Delta is going to be able to use the ADE pathway in the near future, when Wuhan era antibodies will no longer be able to neutralize a mutated Delta strain.
To sum that all up in simpler language, it basically says that Delta is more infectious because it is partially using the ADE method of infection. Future versions may be less prone to be neutralized by Wuhan antibodies, making them fully enhanced. If this happens, we may have more severe disease in those who get infected with this new enhanced Delta.
They conclude by saying a booster against the Wuhan strain will not be effective in improving protection from Delta, and that a new vaccine against Delta will be required.
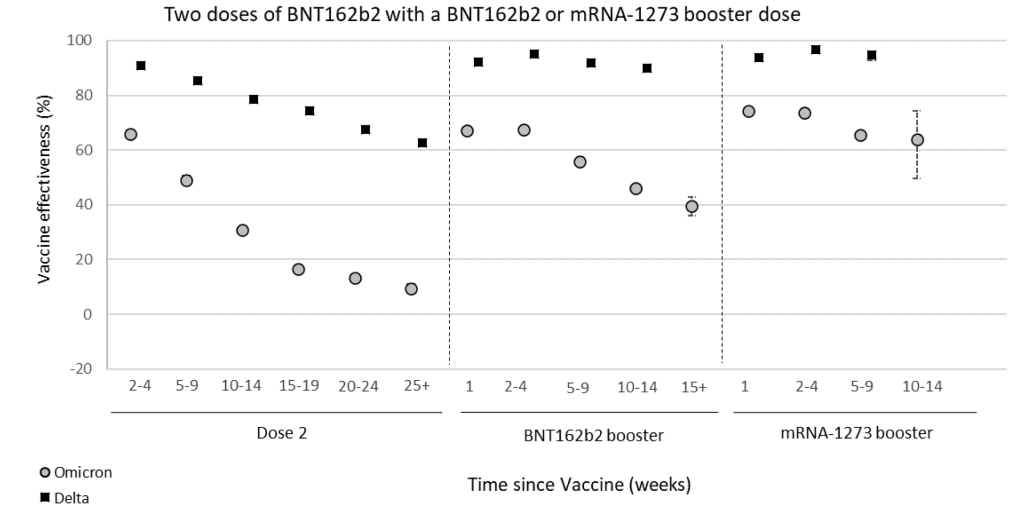
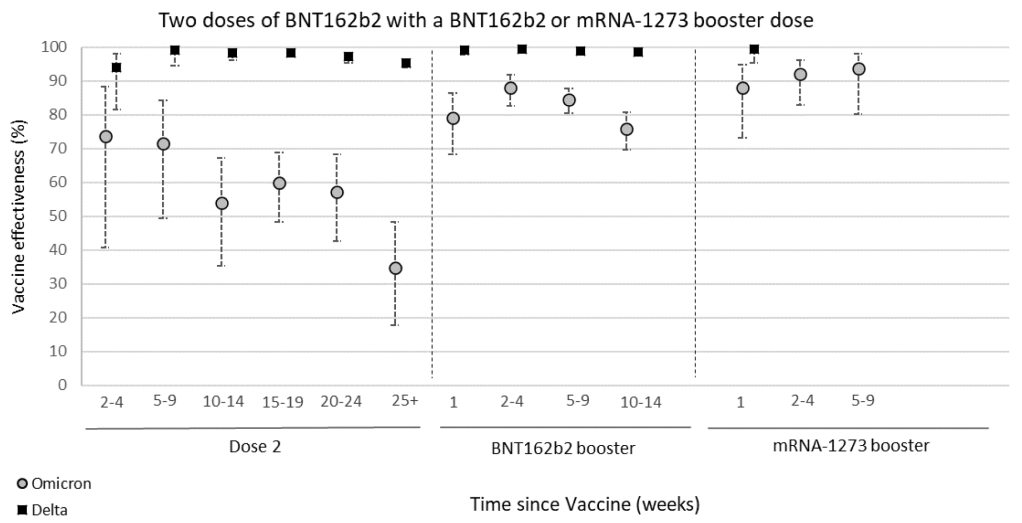
The material in the paper may help to explain why we have been seeing lowering levels of vaccine effectiveness in some countries.
Just to be very clear, they are not saying that this new enhanced Delta exists now, just that it may exist in the future.
I will pay close attention to this issue. If you have already been vaccinated or had COVID, a new Delta vaccine will be your best defense against possible ADE arising from a possible enhanced Delta.
If an enhanced Delta arises, and you have had Wuhan COVID or a Wuhan vaccine, and you haven’t had Delta, then you may be at greater risk for severe disease.
If you have had COVID since July 2021, you are likely already immune to the Delta variant, and this will not be an issue for you.
I am fully aware this complicated. Also, the CDC has rarely if ever discussed this possibility, so unfortunately, most of the people you talk to about this will not believe it. I am sharing this with you so you can make wise decisions for you and your family.
Some companies are already working on Delta versions of the vaccine. If you have had the current vaccines, or had COVID, you should get the Delta vaccines as soon as they are available.
Of course, discuss your medical history with your doctor before making medical decisions.
_________________________________
Updated: January 29th, 2022
The “Final” Verdict on Antibody Dependent Enhancement: As most of you know, ADE has been a major concern of mine from almost the beginning. I’m finally willing to give an assessment of how ADE impacted the pandemic. There were a smattering of cases in previously infected people who may have had more severe cases because of possible ADE, but not more than a smattering. It’s also becoming well acknowledged that Omicron infected everyone regardless of vaccination status and may have even preferentially infected vaccinated people. I know MANY people who are double vaxxed and boosted who got Omicron.
All that being said, I never saw any evidence that conclusively suggested that ADE was causing more severe symptoms because of natural or vaccine mediated immunity. In fact, even during Omicron, during which ADE was most likely to be operating, those with previous immunity clearly fared better than those without. Because I think Omicron is the death rattle of the pandemic, I’m willing to say that ADE never became the threat I was concerned about. For this reason, IF I didn’t already have natural immunity because of Omicron, I might actually get vaccinated IF I could find someone who would aspirate before injecting (see the post from earlier this week)!
I never saw any paper that dealt with the issue of ADE, not even a little. Those that mentioned it did so only in passing.
__________________________________
Updated March 25, 2022
Certain vaccinated individuals are more likely to be infected by Omicron than the unvaccinated: A UK surveillance report shows that vaccine effectiveness against symptomatic Omicron infection goes from around 65% effective soon after 2 doses of vaccine, to around 5% 6 months later. Protection from hospitalization goes down to just 35% after 6 months. These findings suggest that to maintain full protection against Omicron, a vaccinated person will need to get a booster every 3 to 6 months.
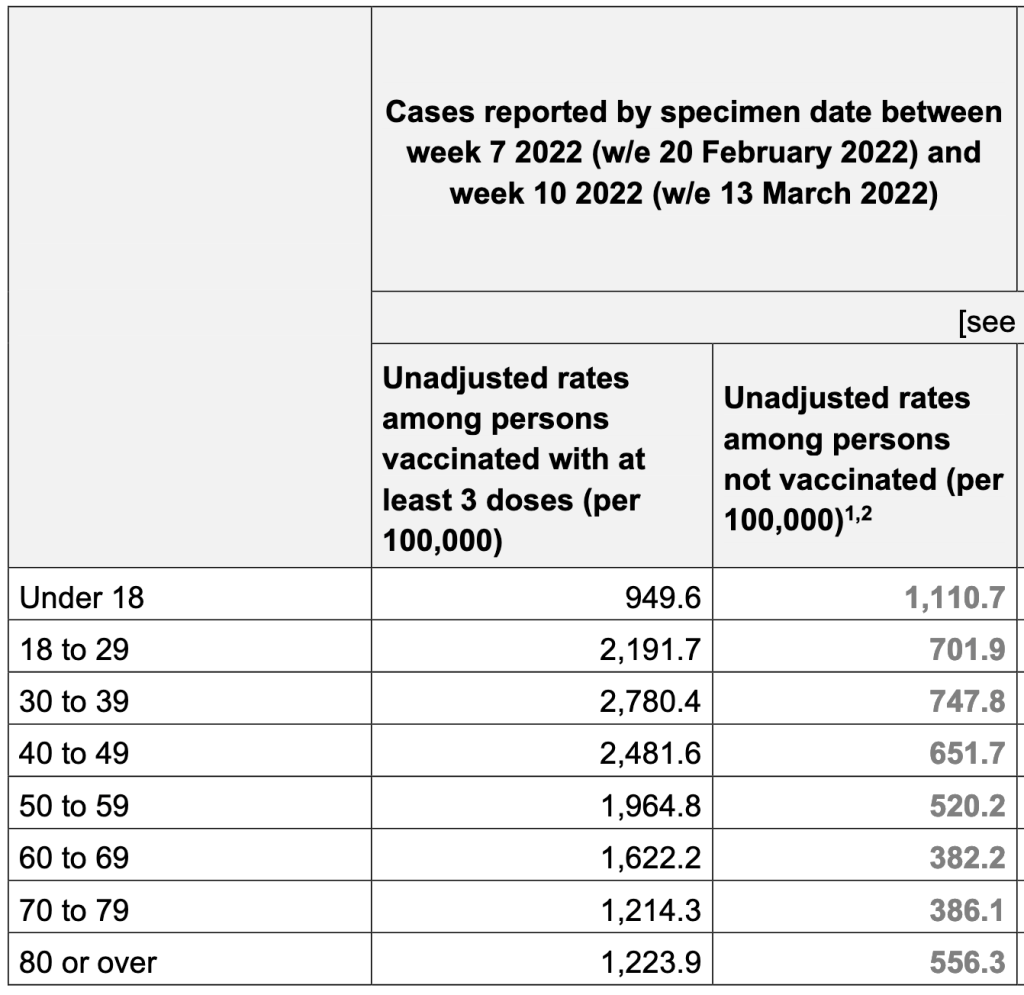
In another finding from the report, people with 3 doses of vaccine are 3x more likely to be infected with Omicron than unvaccinated individuals. This is the clearest evidence yet that Omicron may be using Antibody Dependent Enhancement (ADE) to infect people. The Lewnard et al paper from a few months ago has a similar finding. For both studies, a certain number of vaccine doses are more likely to increase the chance of infection. If viruses are using the ADE pathway, this effect would be explained more by the timing than by the number of doses per se. For ADE to work, a person needs to have a mediocre immune response to an agent, not a strong or weak one. Since we know vaccine mediated immunity goes down over time, then a person becomes more likely to be reinfected as their immune response goes from strong to mediocre.
So should you get a booster? Again, if you have risk factors like age, obesity or respiratory problems, you might want to get a booster every 3 – 6 months. Otherwise, you may choose instead to just take extra precautions as Omicron cases continue to fall in the US. If you choose to get a booster, ask them to aspirate before injection. Talk to your doctor when making medical decisions.
________________________________________________
More than ever, don’t fear, but be smart,
Erik
A selection of relevant papers:
ADE and it’s potential impact for SARS-2:ade-and-sars-2 Download
ADE in SARS-1:ADE and SARS-1 Download
Overlapping symptoms for SARS, MERS, and SARS-2:ade-sars-mers-sars-2-liu_et_al-2020-journal_of_medical_virology Download
Is COVID-19 receiving ADE from other coronaviruses?ADE_and_COVID Download
Possible mechanism for ADE:ade-mechanism-jvi.02015-19 Download