In yesterday’s post, I outlined some of the factors that resulted in the very high COVID case rate in the US. Today I will discuss how we can prepare for the next pandemic.
I have a PhD in molecular biology, and I specialize in infectious disease testing. I am not a physician or epidemiologist. I have an informed but not expert opinion.
Identifying the threat:
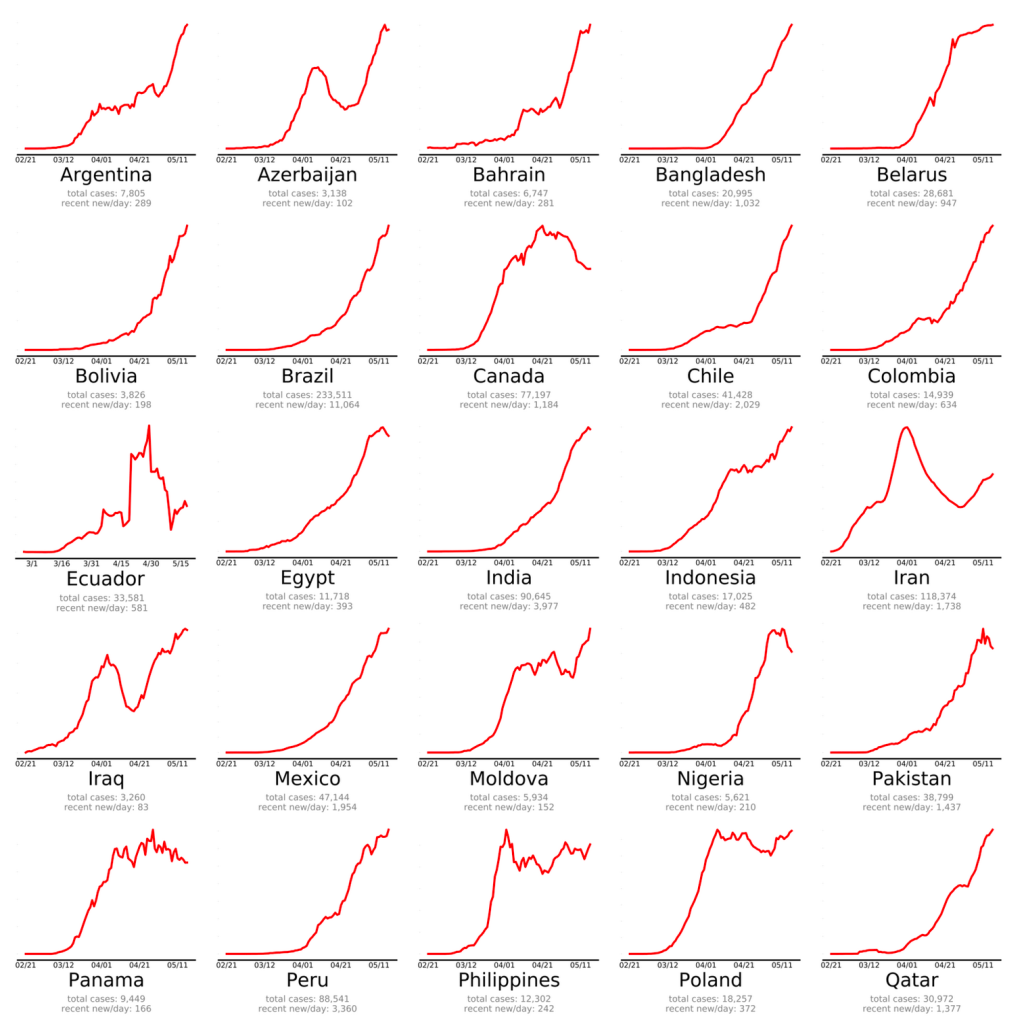
First, most new infectious diseases do not pose a global threat. SARS-2 was so dangerous because of its high infectivity, long incubation time, and asymptomatic spread. Most diseases do not have these parameters. Whenever a new disease comes around, and they will, we should soberly and cautiously assess the real threat. Coming to the wrong conclusions about the threat will lead to the wrong conclusions about combating it.
There have been several important new infectious disease outbreaks in the last few years, including Hantavirus (1993), SARS (2003), Avian Influenza (2004), H1N1 Swine Flu (2009), Ebola (2013), Zika (2015), and of course HIV in the 80s. They all have different disease parameters which make them behave very differently. Most of these diseases did not have global impact. The first SARS for example was much less infectious than SARS-2, but much deadlier, so it was contained quickly and didn’t spread much beyond Asia. HIV can be spread by asymptomatic victims for a full 8-10 years, avoids the immune system, and evades vaccination efforts, so it has become endemic in much of the world.
The following parameters determine how a new disease will behave:
- Mechanism of spread
- Infectivity
- Asymptomatic/ambulatory spread – can the victim walk around and spread disease?
- Incubation period
- Fatality rate
- Vector – what carries the virus to a new host
- Non-human reservoir – diseases that come from non-humans are harder to control and cannot be eradicated.
Obviously, we cannot respond to different diseases in the same way. Part of the reason we failed to contain the virus was that we used measures that were designed for viruses that spread by droplet transmission against a virus that spreads through aerosol transmission. Using the wrong measures was less effective.
Much of my concern with the SARS-2 virus was the Antibody Dependent Enhancement issue, which is very uncommon among viruses, so is not usually a concern.
Be cautious.
Whenever a new threat arises, it is wise to be extra cautious until information can be gathered. Although many of our precautions turned out to be unnecessary, I still support taking extra precautions early on. Remember that early estimates were that the fatality rate for COVID was 3.68%. With the 82 million confirmed cases in the US, this would have been over 3 million deaths if the fatality rate had really been this high. As it stands, we have had almost 1 million COVID related deaths, a death rate of approximately 1.2%. Yes, I know we can debate how many of these are deaths really resulted from COVID and how many infections there really were. But we cannot discount that COVID had an enormous impact.
What if COVID were deadlier? Or what if it had selectively killed children, or caused more long-term symptoms like polio did? Things would have been much different.
All this to say, I think caution was warranted in the beginning of COVID, and we should continue to be cautious in future pandemics. On the other hand, we should also learn to abandon precautions that are not effective. Maintaining ineffective precautions wastes resources, causes extra economic and social suffering, and causes people to lose confidence in government agencies. It started to become clear to me by May of 2020 that lockdowns were ineffective, and that transmission was happening mostly indoors, but I still see people wearing masks outside to this very day.
Persuasion, not coercion:
From the beginning of the pandemic, public communication was terrible. Official guidelines were confusing and often contradictory. Far worse, explanation or evidence was rarely given for policies. Instead, disagreement was met with accusations of being anti-science, rather than persuasion. This approach contributed to the loss in confidence in official channels.
Going forward, officials need far better communication skills when dealing with emergencies. Give evidence rather name-calling, and respect the population enough to tell the whole truth.
Then came the vaccine mandates. Many people I know were coerced into getting vaccinated against their will, and many others were fired. All at a time when information about the vaccines was being hidden from the public. This is unacceptable, and no way to run an emergency.
Here is a link to my post on science communication:
Restoring Trust:
Both the CDC and FDA hid information from the public. In order to restore confidence, senior leadership needs to be replaced and new leadership should explain how things will be better in the future. Is likely to happen? No, it is not.
Government agencies need to be far more transparent. Lack of transparency forces people to wonder what is going on, and create their own theories. Government agencies often decry conspiracy theories, but they had a big role in creating them.
Misinformation:
Freedom of speech, censorship, and misinformation had a major role in the public discussion over the pandemic. Doctors and scientists were frequently censored, shunned, or fired for sharing ideas that went against WHO or CDC guidelines. This includes ideas like the lab leak hypothesis that later turned out to be likely.
Freedom of speech is a foundational principle of American life. It’s in our DNA, as some would say. We are not America without it. Some will say that too much freedom of speech leads to misinformation and conspiracy theories. While it’s true that this freedom allows the spread of falsehoods, it also allows all ideas to be debated, true ideas to be raised up, and false ideas to be discredited. Freedom of speech is the solution to misinformation, not the cause. Most of the leaders in world history that wanted to control freedom of speech had something to hide. It is essential that we maintain this basic right.
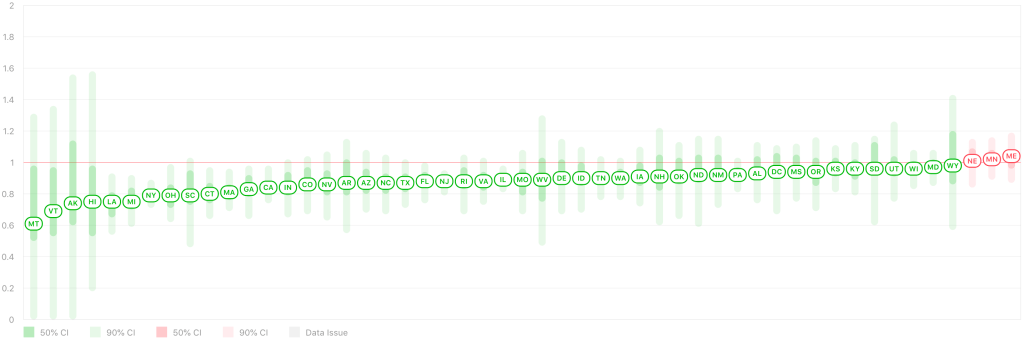
State emergency powers:
As discussed in yesterday’s post, the US federal government has surprisingly little power to deal with a public health crisis. The CDC can develop guidelines, but most of the real work is done at the state and local level. State officials need to step up and realize it’s their responsibility to respond well. Citizens need to hold state and local officials accountable.
Manufacturing:
The US needs to maintain manufacturing capacity for certain essential items like personal protective equipment, testing kits and equipment, and medications. Tax incentives need to exist to encourage companies not to send these functions overseas.
In addition, we should have national and state stockpiles of certain equipment. I know many hospitals and labs are now creating stockpiles of their own.
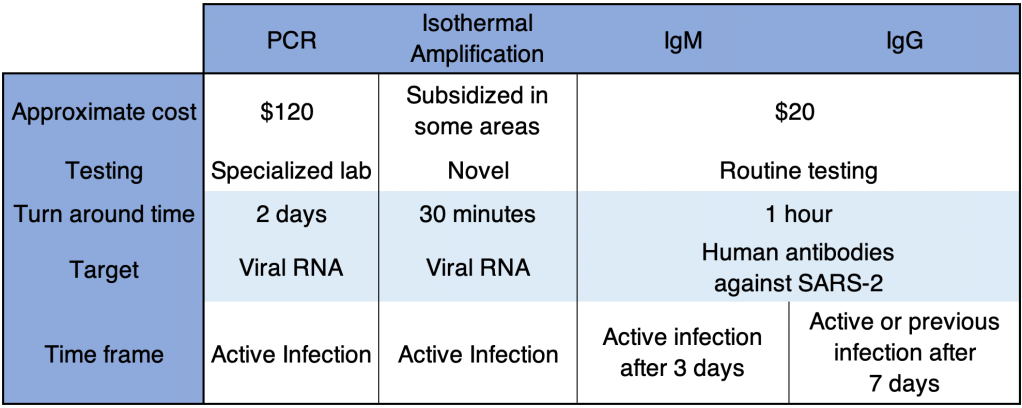
Testing:
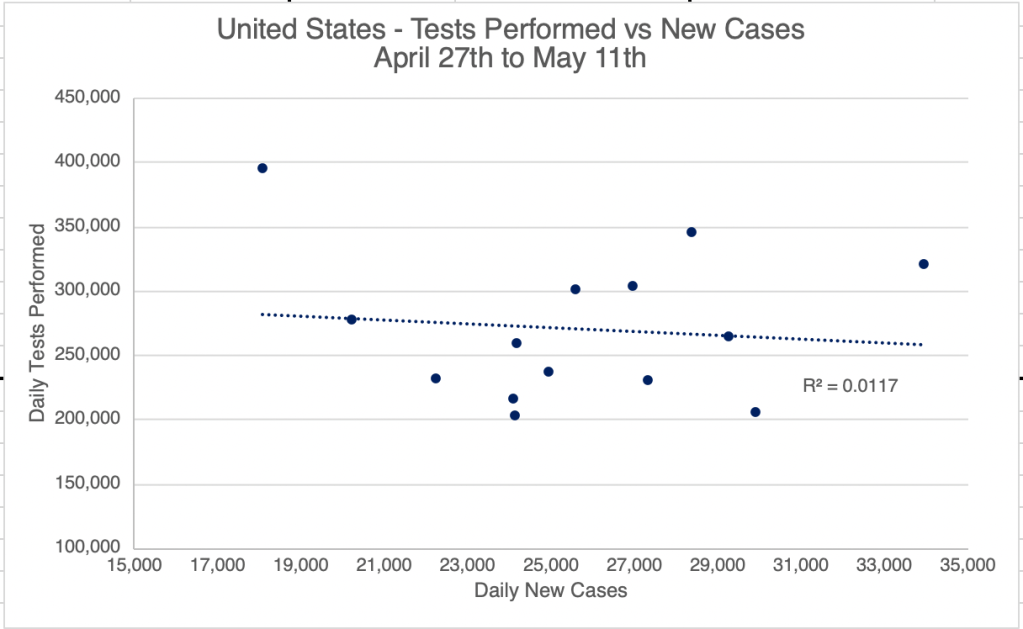
Most countries that did well produced lots of COVID testing early. In the US, the CDC tried to manage all the testing themselves, and quickly became overwhelmed. By the time private labs were allowed to develop their own tests, it was way too late. Testing capacity didn’t become nearly adequate until at least July of 2020. Next time, the CDC needs to allow testing by private labs right away. Ideally, anyone who wants a test and anyone potentially exposed to an agent should be tested.
Quarantine, not Lockdown:
Countries that did well did not quarantine healthy individuals, although some of these countries had more restrictions during the big Winter waves. Instead, only COVID positive people should be quarantined. This is only effective when tests are readily available.
Later in the pandemic, some outlets acknowledged that most infections were happening in private settings. Basically, people would get infected outside, then bring COVID home to infect everyone in the household.
Here is a very interesting video using computer models to show why our model of lockdown was not effective. Computer models are only as good as they are programmed to be, so this is only for demonstration purposes, and is not data.
Contact tracing:
Contact tracing was very successful in some countries, but the long incubation time of COVID made this difficult. Successful programs involved tracking of individuals by cell phone and credit card data, practices that would probably not be tolerated in the US. Such programs would need to be voluntary to not trigger the creepiness factor and violate constitutional rights.
Masking:
I was a big proponent of wearing a medical grade respirator (N95, KN95, or KN94) indoors during the pandemic. Because COVID spread as an aerosol as well as droplet form, cloth and blue surgical masks were ineffective. Simpler masks can be effective against colds and flu, however. So the choice of mask depends on the agent in question. CDC guidelines need to reflect the method of spread of the agent in question.
So what should Dr. Fauci have said early on? Something like this:
“N95 masks offer the best protection against infection by the SARS-2 virus. However, our current supply is very low, and we desperately need to save these masks for our medical professionals. Please do not purchase N95 masks at this time. In the mean time, there are some options that will help reduce the risk…”
In actuality, of course, I didn’t see an N95 in a store from March 2020 until at least February of 2021, so I couldn’t have bought one if I’d wanted to!
Treatment:
Most medical facilities in the US didn’t treat COVID until a patient was experiencing respiratory distress. By then, treatment options were limited. To their credit, intubation was largely abandoned by the medical community when it was learned that this treatment was largely ineffective.
However, controversy swirled over potential treatments that became disfavored by the medical community. Doctors are usually granted the right to prescribe “off label” medications, meaning they can use medications for treatments outside the guidelines of the manufacturer. But drugs like Hydroxychloroquine, Ivermectin, and others quickly become forbidden, and some doctors even got fired for prescribing them. Research on these drugs were minimal.
I am not arguing here that these drugs are effective against COVID. I’m simply saying that forbidding doctors from working with or publishing papers about these drugs was a big mistake. While it is of course wise for a doctor to consider guidelines, treating a novel virus may require some “outside the box” thinking.
Let me know in the comments if I missed something important!
Don’t fear, but be smart!
Erik